Alternative Names: Legg-Calve-Perthes’ disease, ischemic necrosis of the hip, coxa plana, osteochondritis and avascular necrosis of the femoral head, Legg–Perthes Disease or Legg–Calve-Perthes Disease (LCPD).
Definition:
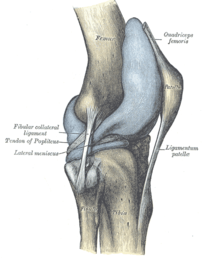
Perthes’ disease is a degenerative disease of the hip joint, where growth/loss of bone mass leads to some degree of collapse of the hip joint and to deformity of the ball of the femur and the surface of the hip socket. The disease is characterized by idiopathic avascular osteonecrosis of the capital femoral epiphysis of the femoral head leading to an interruption of the blood supply of the head of the femur close to the hip joint. The disease is typically found in young children, and it can lead to osteoarthritis in adults. The effects of the disease can sometimes continue into adulthood.
Perthes’ disease affects the top of the femur (thigh bone) where it meets the hip bone. The blood supply to the growth plate of the bone (epiphysis) becomes inadequate. As a result, the bone softens and breaks down – a process called necrosis.
This happens gradually over several weeks. Then, as the blood supply recovers, the bone reforms and hardens. This takes 18 to 36 months and may lead to a deformed shape, with flattening of the ball-shaped head of the femur that normally fits into the round socket of the hip joint.
Recent research has suggested Perthes’ may be linked to a subtle problem with blood clotting.
Perthes’ most commonly affects children between the ages of four and eight, but younger children and teenagers can also develop the condition.
It affects around one in 20,000 children and is up to five times more common in boys. It’s also more common among Caucasians.
In ten to 20 per cent of cases, both hips are affected.
It is named for Arthur Legg, Jacques Calvé and Georg Perthes and was first described by Karel Maydl.
:
Symptoms:
The first symptom is often limping, which is usually painless. Sometimes there may be mild pain that comes and goes.
Other symptoms may include:
•Hip stiffness that restricts movement in the hip
•Knee pain
•Limited range of motion
•Persistent thigh or groin pain
•Shortening of the leg, or legs of unequal length
•Wasting of muscles in the upper thigh
Causes:
Legg believed trauma to be the cause, Calve ricketts, and Perthes infection. Presently, a number of factors have been implicated including heredity, trauma, endocrine, inflammatory, nutritional, and altered circulatory hemodynamics.
Although no-one has identified the cause of Perthes disease it is known that there is a reduction in blood flow to the joint. It is thought that the artery of the ligamentum teres femoris closes too early, not allowing time for the medial circumflex femoral artery to take over. For example, a child may be 6 years old chronologically but may have grown to 4 years old in terms of bone maturity. The child may then engage in activity appropriate for a child of 6 but may not yet have the bone strength of an older child, leading to flattening or fracture of the hip joint. Genetics do not appear to be a determining factor, but it has been suggested that a deficiency of some blood factors used to disperse blood clots may lead to blockages in the vessels supplying the joint, but these have not been proven. There is also a deficiency of proteins C and S which act as blood anticoaglants and their deficiency may cause clot formation in ligamentum teres femoris artery and hinder blood supply to the femoral head
Risk factors:
Perthes disease can affect children of nearly any age, but it’s most common among boys ages 2 to 12. In fact, it’s up to five times more common in boys. When girls develop Legg-Calve-Perthes disease, it tends to be more severe.
In addition, Perthes disease is most common in Asians, Eskimos and whites. The disease may be more likely in physically active children who are small for their age and in those who are exposed to secondhand smoke.
Complications:
*Permanent hip deformity. Perthes disease may cause a permanently deformed hip joint — especially if the condition develops after ages 6 to 8.
*Osteoarthritis may develop later in life. Early recognition and proper treatment of Perthes disease may minimize this complication.
Diagnosis:
X-Rays of the hip confirm the diagnosis. X-rays usually demonstrate a flattened, and later fragmented, femoral head. A bone scan or MRI may be useful in making the diagnosis in those cases where x-rays are inconclusive. Neither bone scan nor MRI offer any additional useful information beyond that of x-rays in an established case. If MRI or bone scans are necessary, a positive diagnosis relies upon patchy areas of vascularity to the capital femoral epiphysis (the developing femoral head).
Treatment :
The goal of treatment is to keep the ball of the thighbone inside the socket and to avoid severe degenerative arthritis. Your health care provider may call this “containment.”
Physical therapy and anti-inflammatory medicine (such as ibuprofen) can relieve stiffness in the hip joint. When the hip is painful, or the limp gets worse, restricting activities such as running may help reduce the inflammation. Nighttime traction may also help.
Health care providers no longer recommend several months of bedrest.
Orthopedic assessment is crucial. Younger children have a better prognosis than older children.
Treatment has traditionally centered on removing pressure from the joint until the disease has run its course. Options include traction (to separate the femur from the pelvis and reduce wear) braces (often for several months, with an average of 18 months) to restore range of motion, physiotherapy, and surgical intervention when necessary because of permanent joint damage. To maintain activities of daily living, custom orthotics may be used. These devices internally rotate the femoral head and abduct the leg(s) at 45 degrees. Orthoses can start as proximal as the lumbar spine (LSO), and extend the length of the limbs to the floor. Most functional bracing is achieved using a waist belt and thigh cuffs derived from the Scottish-Rite Orthosis. These devices are typically prescribed by a physician and implemented by a certified orthotist. For older children, the distraction method has been found to be a successful treatment, using an external fixator which relieves the hip from carrying the body’s weight. This allows room for the top of the femur to regrow. Many children need no intervention at all and are simply asked to refrain from contact sports or games which impact the hip. The Perthes Association has a “library” of equipment which can be borrowed to assist with keeping life as normal as possible, newsletters, a helpline, and events for the families to help children and parents to feel less isolated.
Modern treatment focuses on removing pressure from the joint to increase blood flow, in concert with physiotherapy. Pressure is minimized on the hip through use of crutches or a cane, and the avoidance of running-based sports. Swimming is highly recommended, as it allows exercise of the hip muscles with full range of motion while reducing the stress to a minimum. Cycling is another good option as it also keeps stress to a minimum. Physiotherapy generally involves a series of daily exercises, with weekly meetings with a physiotherapist to monitor progress. These exercises focus on improving and maintaining a full range of motion of the femur within the hip socket. Performing these exercises during the healing process is essential to ensure that the femur and hip socket have a perfectly smooth interface. This will minimize the long term effects of the disease. Use of zoledronic acid has also been investigated.
Perthes disease is self limiting, but if the head of femur is left deformed there can be a long-term problem. Treatment is aimed at minimizing damage while the disease runs its course, not at ‘curing’ the disease. It is recommended not to use steroids or alcohol as these reduce oxygen in the blood which is needed in the joint. As sufferers age, problems in the knee and back can arise secondary to abnormal posture and stride adopted to protect the affected joint. The condition is also linked to arthritis of the hip, though this appears not to be an inevitable consequence. Hip replacements are relatively common as the already damaged hip suffers routine wear; this varies by individual, but generally is required any time after age 50.
Prognosis:
The Prognosis depends on the child’s age and the severity of the disease. In general, the younger the child is when the disease starts, the better the outcome.
Children younger than 6 have the best prognosis since they have time for the dead bone to revascularize and remodel, with a good chance that the femoral head will recover and remain spherical after resolution of the disease. Children who have been diagnosed with Perthes’ Disease after the age of 10 are at a very high risk of developing osteoarthritis and Coxa Magna.
Disclaimer: This information is not meant to be a substitute for professional medical advise or help. It is always best to consult with a Physician about serious health concerns. This information is in no way intended to diagnose or prescribe remedies.This is purely for educational purpose
Resources:
http://www.nlm.nih.gov/medlineplus/ency/article/001264.htm
http://en.wikipedia.org/wiki/Legg%E2%80%93Calv%C3%A9%E2%80%93Perthes_syndrome
http://www.mayoclinic.com/health/legg-calve-perthes-disease/DS00654
http://www.bbc.co.uk/health/physical_health/conditions/perthes2.shtml
http://orthoinfo.aaos.org/topic.cfm?topic=A00070
http://www.concordortho.com/patient-education/topic-detail-popup.aspx?topicID=8de6c8d126950dbbae6601bda872854b
Related articles
- McMinn Centre (UK) Talks About Arthritis (earlsview.com)
- IBD, LCPD health research in ‘Westie’ dogs may hold answers to similar human diseases (eurekalert.org)
- Is My Hip Replacement Hurting? (everydayhealth.com)
- A Guide to Hip Anatomy (everydayhealth.com)
- How Common Is Hip Replacement? (everydayhealth.com)
- Mr. Michael Solomon, Sydney Australia Surgeon Gives Advice on Hip Replacement (earlsview.com)
- Clive Bingwa and Derry Simpson elected to 303?s board (mumbrella.com.au)
- Paget’s Disease of Bone (findmeacure.com)
- Effects of celiac disease on bone mineral density are pronounced in lumbar spine than femoral neck (eurekalert.org)
- Hip Pain: What Do Your Symptoms Mean? (everydayhealth.com)



![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)