Alternative Name: Diverticulosis…………..click for picture
Definition:
Over a lifetime, it’s estimated the human gut digests more than 65 tonnes of food and drink. Much of this food will be low in fibre, putting the gut under strain.
One common outcome of this is diverticular disease, a condition affecting the large bowel, or colon, believed to be the result of too little fibre in the diet.
A diet low in fibre creates the ideal conditions for constipation to develop. When this happens, the pressure in the large part of the gut increases, which forces small parts of the gut lining outwards through the muscles surrounding the gut. This causes the lining to form small balloon-like pouches called diverticula..
Diverticula are pockets that develop in the colon wall, usually in the sigmoid or left colon, but may involve the entire colon. Diverticulosis describes the presence of these pockets. Diverticulitis describes inflammation or complications of these pockets.
About one in two adults over 50 is affected, and most adults are affected by the time they reach 80 to 90. Men and women are affected equally.
Diverticular disease is very uncommon in countries such as Africa, where diets are high in fibre. In Western countries, where many people still don’t eat enough fibre, it becomes more common as people get older.
Symptoms:
Signs and symptomsMost people with colonic diverticulosis are unaware of this structural change. When symptoms do appear in a person over 40 years of age it is important to obtain medical advice and exclude more dangerous conditions such as cancer of the colon or rectum.
The clinical forms of colonic diverticulosis are
*Symptomatic colonic diverticulosis………..click to see the picture
This is the most common complication of colonic diverticulosis. This is when the motility (that is, the onward propulsive nature of contractions) of the bowel becomes disorganized. Sometimes, spasm can develop. This results in pain in the left lower abdomen and often is accompanied by the passage of small pelletty stools and slime which relieves the pain. Symptoms can consist of (1) bloating, (2) changes in bowel movements (diarrhea or constipation), (3) Non-specific chronic discomfort in the lower left abdomen, with occasional acute episodes of sharper pain, (4) abdominal pain, often aftick to see the pictureer meals often in the left lower abdomen. If these persist clinical investigation is advised.
*Complicated colonic diverticulosis
This is very uncommon but highly dangerous. The diverticulae may bleed, either rapidly (causing bleeding through the rectum) or slowly (causing anaemia). The diverticulae can become infected and develop abscesses, or even perforate. These are serious complications and medical care is needed. Infected diverticulae and development of abscesses merits the term diverticulitis. First time bleeding from the rectum, especially in individuals aged over age 40, could be due to colon cancer, colonic polyps and inflammatory bowel disease rather than diverticulosis and requires clinical investigation.
Infection in the diverticula, possibly caused by an impacted piece of faeces, is responsible for the inflammation that develops. When this happens – called diverticulitis – the pain is very severe and usually felt in the lower left side of the abdomen.
A person will often feel feverish and have nausea and vomiting. They may pass blood rectally.
Risk factors:
1.increasing age
2.constipation
3.a diet that is low in dietary fiber content or high in fat
4.high intake of meat and red meat
5.connective tissue disorders (such as Marfan syndrome) that may cause weakness in the colon wall.
The exact aetiology of colonic diverticulosis has yet to be fully clarified and many of the claims are only anecdotal. The modern emphasis on the value of fiber in the diet began with Cleave. A strong case was made by Neil Painter and Adam Smith that a deficiency of dietary fiber is the cause of diverticular disease. They argued that the colonic muscles needed to contract strongly in order to transmit and expel the small stool associated with a fiber deficient diet. The increased pressure within the segmented section of bowel over years gave rise to herniation at the vulnerable point where blood vessels enter the colonic wall. Denis Burkitt had suggested that the mechanical properties of the colon may be different in the African and the European subjects. Because Africans eat a diet containing much more fiber than Europeans and use the natural squatting position for defecation, they pass bulky stools, and hence rarely if ever develop colonic diverticulosis. The US National Institutes of Health (NIH) considers the fiber theory “unproven.”
However, change in the strength of the colonic wall with age may be an aetiological factor. Connective tissue is a significant contributor to the strength of the colonic wall. The mechanical properties of connective tissue depend on a wide variety of factors, the type of tissue and its age, the nature of the intramolecular and intermolecular covalent cross links and the quantity of the glycosaminoglycans associated with the collagen fibrils. The submucosa of the colon is composed almost entirely of collagen, both type I and type III. Several layers of collagen fibres make up the submucosa of the human colon. The collagen fibril diameters and fibril counts are different between the left and right colon and change with age and in colonic diverticulosis,. The implication being that changes which are normally associated with ageing are more pronounced in colonic diverticulosis. Iwasaki found that the tensil strength of the Japanese colon obtained at postmortem declined with age. Similarly the mechanical properties of the colon are stronger in African than European subjects. However, this race-based claim is contradicted by the virtually identical incidence of diverticular disease in black and white Americans.
The strength of the colon decreases with age in all parts of the colon, except the ascending colon. The fall in tensile strength with age is due to a decrease in the integrity of connective tissue. Cross linkage of collagen is increased in colonic diverticulosis. The mucosal layer is possibly more elastic and it is likely that the stiffer external layers break and allow the elastic mucosa to herniate through forming a diverticulum. Collagen has intermolecular and intramolecular cross links which stabilise and give strength to the tissue in which it is located. Accumulation of covalently linked sugar molecules and related increasing cross linking products are found in a variety of tissues with ageing, skin, vascular tissue, the cordae tendinae of heart valves and the colon. This reduces the strength and pliability of the collagen. Colonic diverticulosis increases in frequency with age. There is a reduction in the strength of the colonic mucosa with age, and that increased contractions in the descending and sigmoid colon secondary to an insufficient fibre content of the diet cause protrusion through this weakened wall. Colonic diverticulosis is in general a benign condition of the bowel which uncommonly becomes symptomatic and even less commonly becomes a truly clinical complicated problem.
Diagnosis:
In cases of asymptomatic Diverticulosis, the diagnosis is usually made as an incidental finding on other investigations.
While a good history is often sufficient to form a diagnosis of Diverticulosis or Diverticulitis, it is important to confirm the diagnosis and rule out other pathology (notably colorectal cancer) and complications.
Investigations:-
*Plain Abdominal X-ray may show signs of a thickened wall, ileus, constipation, small bowel obstruction or free air in the case of perforation. Plain X-rays are insufficient to diagnose Diverticular Disease.
*Contrast CT is the investigation of choice in acute episodes of Diverticulitis and where complications exist.
*Colonoscopy will show the diverticulum and rule out malignancy. A Colonoscopy should be performed 4–6 weeks after an acute episode.
*Barium enema is inferior to colonoscopy in terms of image quality and is usually only performed if the patient has strictures or an excessively tortuous sigmoid colon where colonoscopy is difficult or dangerous.
*MRI provides a clear picture of the soft tissue of the abdomen, however its expense often outweighs the benefits when compared to contrast CT or colonoscopy.
*There is no blood test for Diverticulosis.
It is important to note that both Barium enema and Colonoscopy are contraindicated during acute episodes of diverticulitis.
Management & Treatment:
Many patients with diverticulosis have minimal or no symptoms, and do not require any specific treatment. A high-fiber diet and fiber supplements are advisable to prevent constipation . The American Dietetic Association recommends 20-35 grams each day. Wheat bran has much to commend it as this has been shown to reduce intra colonic pressure Ispaghula is also effective at 1-2 grams a day. Colonic stimulants should be avoided. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) says foods such as nuts, popcorn hulls, sunflower seeds, pumpkin seeds, caraway seeds, and sesame seeds have traditionally been labelled as problem foods for people with this condition; however, no scientific data exists to prove this hypothesis. The seeds in tomatoes, zucchini, cucumbers, strawberries, raspberries, and poppy seeds, are not considered harmful by the NIDDK. Treatments, like some colon cleansers, that cause hard stools, constipation, and straining, are not recommended. Some doctors also recommend avoidance of fried foods, nuts, corn, and seeds to prevent complications of diverticulosis. Whether these diet restrictions are beneficial is uncertain; recent studies have stated that nuts and popcorn do not contribute positively or negatively to patients with diverticulosis or diverticular complications. When the spasm pain is troublesome the use of peppermint oil (1 drop in 50 ml water), or peppermint tablets (e.g., colpermin), can be helpful. Complicated diverticulosis requires treatment of the complication. These complications are often grouped under a single diagnosis of diverticulitis and require skilled medical care of the infection, bleeding and perforation which may include intensive antibiotic treatment, intravenous fluids and surgery. Complications are more common in patients who are taking NSAIDS or aspirin. As diverticulosis occurs in an older population such complications are serious events.
Someone with diverticulitis may be treated at home with painkillers, antibiotics, laxatives and dietary advice. But diverticulitis is often severe, and can need hospital treatment with antibiotics and fluids given through a drip.
In some cases, the bowel may perforate, become obstructed or bleed heavily. When this happens, the situation becomes an emergency and an operation may be needed.
Surgery is reserved for patients with recurrent episodes of diverticulitis, complications or severe attacks when there’s little or no response to medication. Surgery may also be required in individuals with a single episode of severe bleeding from diverticulosis or with recurrent episodes of bleeding.
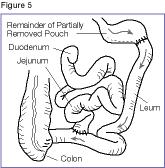
Surgical treatment for diverticulitis removes the diseased part of the colon, most commonly, the left or sigmoid colon. Often the colon is hooked up or “anastomosed” again to the rectum. Complete recovery can be expected. Normal bowel function usually resumes in about three weeks. In emergency surgeries, patients may require a temporary colostomy bag. Patients are encouraged to seek medical attention for abdominal symptoms early to help avoid complications.
Complications:
Infection of a diverticulum can result in diverticulitis. This occurs in 10-25% of persons with diverticulosis (NIDDK website). Tears in the colon leading to bleeding or perforations may occur; intestinal obstruction may occur (constipation or diarrhea does not rule this possibility out); and peritonitis, abscess formation, retroperitoneal fibrosis, sepsis, and fistula formation are also possible occurrences. Rarely, an enterolith may form.
Low fiber, high fat diet, constipation and use of stimulant laxatives increase the risk of bleeding, also history of diverticulitis increases the chance to bleed.
Infection of a diverticulum often occurs as a result of stool collecting in a diverticulum.
More than 10% of the US population over the age of 40 and half over the age of 60 has diverticulosis. This disease is common in the US, Britain, Australia, Canada, and is uncommon in Asia and Africa . Large-mouth diverticula are associated with scleroderma.
Disclaimer: This information is not meant to be a substitute for professional medical advise or help. It is always best to consult with a Physician about serious health concerns. This information is in no way intended to diagnose or prescribe remedies.This is purely for educational purpose.
Resources:
http://www.bbc.co.uk/health/physical_health/conditions/diverticulardisease1.shtml
http://en.wikipedia.org/wiki/Diverticulosis
http://www.fascrs.org/patients/conditions/diverticular_disease/
http://www.procto-med.com/images/2009/05/diverticular-disease.gif
http://www.advgastro.com/diverticulitis.htm
Related articles
- The Diverticular Disease Diet (everydayhealth.com)
- Questions to Ask Your Doctor About Diverticulosis (everydayhealth.com)
- What is diverticulosis? (zocdoc.com)
- Two of a Kind? (everydayhealth.com)
- What is diverticulits crohn disease (wiki.answers.com)
- What’s the difference between Diverticulosis and Diverticulitis (mirror.co.uk)
- Signs and Symptoms of Colon Polyps (brighthub.com)



![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)































