ntroduction:
Most people have had a minor knee problem at one time or another. Most of the time our body movements do not cause problems, but it’s not surprising that symptoms develop from everyday wear and tear, overuse, or injury. Knee problems and injuries most often occur during sports or recreational activities, work-related tasks, or home projects..
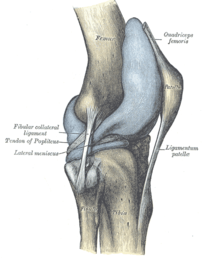
The knee is the largest joint in the body. The upper and lower bones of the knee are separated by two discs (menisci). The upper leg bone (femur) and the lower leg bones (tibia and fibula) are connected by ligaments, tendons, and muscles. The surface of the bones inside the knee joint is covered by articular cartilage, which absorbs shock and provides a smooth, gliding surface for joint movement. See an illustration of the structures of the knee .
Although a knee problem is often caused by an injury to one or more of these structures, it may have another cause. Some people are more likely to develop knee problems than others. Many jobs, sports and recreation activities, getting older, or having a disease such as osteoporosis or arthritis increase your chances of having problems with your knees.
Sudden (acute) injuries
Injuries are the most common cause of knee problems. Sudden (acute) injuries may be caused by a direct blow to the knee or from abnormal twisting, bending the knee, or falling on the knee. Pain, bruising, or swelling may be severe and develop within minutes of the injury. Nerves or blood vessels may be pinched or damaged during the injury. The knee or lower leg may feel numb, weak, or cold; tingle; or look pale or blue. Acute injuries include:
•Sprains, strains, or other injuries to the ligaments and tendons that connect and support the kneecap.
•A tear in the rubbery cushions of the knee joint (meniscus).
•Ligament tears. The medial collateral ligament (MCL) is the most commonly injured ligament of the knee.
•Breaks (fracture) of the kneecap, lower portion of the femur, or upper part of the tibia or fibula. Knee fractures are most commonly caused by abnormal force, such as a falling on the knee, a severe twisting motion, severe force that bends the knee, or when the knee forcefully hits an object.
•Kneecap dislocation. This type of dislocation occurs more frequently in 13- to 18-year-old girls. Pieces of bone or tissue (loose bodies) from a fracture or dislocation may get caught in the joint and interfere with movement.
•Knee joint dislocation. This is a rare injury that requires great force. It is a serious injury and requires immediate medical care.
CLICK & SEE
Overuse injuries


Overuse injuries occur with repetitive activities or repeated or prolonged pressure on the knee. Activities such as stair climbing, bicycle riding, jogging, or jumping stress joints and other tissues and can lead to irritation and inflammation. Overuse injuries include:
•Inflammation of the small sacs of fluid that cushion and lubricate the knee (bursitis).
•Inflammation of the tendons (tendinitis) or small tears in the tendons (tendinosis).
•Thickening or folding of the knee ligaments (Plica syndrome).
•Pain in the front of the knee from overuse, injury, excess weight, or problems in the kneecap (patellofemoral pain syndrome).
•Irritation and inflammation of the band of fibrous tissue that runs down the outside of the thigh (iliotibial band syndrome).
Conditions that may cause knee problems
Problems not directly related to an injury or overuse may occur in or around the knee.
•Osteoarthritis (degenerative joint disease) may cause knee pain that is worse in the morning and improves during the day. It often develops at the site of a previous injury. Other types of arthritis, such as rheumatoid arthritis, gout, and lupus, also can cause knee pain, swelling, and stiffness.
•Osgood-Schlatter disease causes pain, swelling, and tenderness in the front of the knee below the kneecap. It is especially common in boys ages 11 to 15.
•A popliteal (or Baker’s) cyst causes swelling in the back of the knee.
•Infection in the skin (cellulitis), joint (infectious arthritis), bone (osteomyelitis), or bursa (septic bursitis) can cause pain and decreased knee movement.
•A problem elsewhere in the body, such as a pinched nerve or a problem in the hip, can sometimes cause knee pain.
•Osteochondritis dissecans causes pain and decreased movement when a piece of bone or cartilage or both inside the knee joint loses blood supply and dies.
.Treatment
Treatment for a knee problem or injury may include first aid measures, rest, bracing, physical therapy, medicine, and in some cases surgery. Treatment depends on the location, type, and severity of the injury as well as your age, health condition, and activity level (such as work, sports, or hobbies).
YOU MAY CLICK TO CHECK SYMPTOMS OF EMERGENCY & TAKE ACTION ACCORDINGLY:
Home Treatment
Home treatment may help relieve pain, swelling, and stiffness.

•Rest and protect an injured or sore area. Stop, change, or take a break from any activity that may be causing your pain or soreness. When resting, place a small pillow under your knee.
•Ice will reduce pain and swelling. Apply ice or cold packs immediately to prevent or minimize swelling. Apply the ice or cold pack for 10 to 20 minutes, 3 or more times a day.
*For the first 48 hours after an injury, avoid things that might increase swelling, such as hot showers, hot tubs, hot packs, or alcoholic beverages.
*After 48 to 72 hours, if swelling is gone, apply heat and begin gentle exercise with the aid of moist heat to help restore and maintain flexibility. Some experts recommend alternating between heat and cold treatments.
•Compression, or wrapping the injured or sore area with an elastic bandage (such as an Ace wrap), will help decrease swelling.
*Don’t wrap it too tightly, since this can cause more swelling below the affected area. Loosen the bandage if it gets too tight. Signs that the bandage is too tight include numbness, tingling, increased pain, coolness, or swelling in the area below the bandage.
*Don’t expect the bandage to protect or stabilize a knee injury.
*Talk to your doctor if you think you need to use a wrap for longer than 48 to 72 hours; a more serious problem may be present.
•Elevate the injured or sore area on pillows while applying ice and anytime you are sitting or lying down. Try to keep the area at or above the level of your heart to help minimize swelling.
.
•Reduce stress on your sore knee (until you can get advice from your doctor):
*Use a cane or crutch in the hand opposite your painful knee.
*Use two crutches, keeping weight off the leg with the sore knee. You can get canes or crutches from most pharmacies. Crutches are recommended if a cane causes you to walk with a limp.
•Gently massage or rub the area to relieve pain and encourage blood flow. Do not massage the injured area if it causes pain.
.
•Try the following exercises to maintain flexibility:
*Hamstring stretch *Knee-to-chest exercise •Avoid high-impact exercise, such as running, skiing, snowboarding, or playing tennis, until your knee is no longer painful or swollen.
Do not smoke. Smoking slows healing because it decreases blood supply and delays tissue repair. For more information, see the topic Quitting Tobacco Use.
Medicine you can buy without a prescription Try a nonprescription medicine to help treat your fever or pain: –
.•Acetaminophen, such as Tylenol or Panadol
Note: Do not use a nonsteroidal anti-inflammatory medicine, such as ibuprofen or aspirin, for the first 24 hours after an injury. Using these medicines may increase the time it takes your blood to clot and cause more severe bruising from bleeding under the skin.
.
•Nonsteroidal anti-inflammatory drugs (NSAIDs):
*Ibuprofen, such as Advil or Motrin
*Naproxen, such as Aleve or Naprosyn
•Aspirin (also a nonsteroidal anti-inflammatory drug), such as Bayer or Bufferin
Talk to your child’s doctor before switching back and forth between doses of acetaminophen and ibuprofen. When you switch between two medicines, there is a chance your child will get too much medicine.
Safety tips Be sure to follow these safety tips when you use a nonprescription medicine: –
•Carefully read and follow all directions on the medicine bottle and box.
•Do not take more than the recommended dose.
•Do not take a medicine if you have had an allergic reaction to it in the past.
•If you have been told to avoid a medicine, call your doctor before you take it.
•If you are or could be pregnant, do not take any medicine other than acetaminophen unless your doctor has told you to.
•Do not give aspirin to anyone younger than age 20 unless your doctor tells you to.
.
Symptoms to Watch For During Home Treatment
Use the Check Your Symptoms section to evaluate your symptoms if any of the following occur during home treatment:
•Signs of infection develop.
•Numbness, tingling, or weakness develops.
•Your knee, lower leg, or foot becomes pale or cool or looks blue.
•Symptoms do not improve with home treatment.
•Symptoms become more severe or frequent.
Prevention
The following tips may prevent knee problems.
General prevention tips
•Wear your seat belt in a motor vehicle.
•Don’t carry objects that are too heavy. Use a step stool. Do not stand on chairs or other unsteady objects.
•Wear knee guards during sports or recreational activities, such as roller-skating or soccer.
•Stretch before and after physical exercise, sports, or recreational activities to warm up your muscles.
•Use the correct techniques or positions during activities so that you do not strain your muscles.
•Use equipment appropriate to your size, strength, and ability. Avoid repeated movements that can cause injury. In daily routines or hobbies, look at activities in which you make repeated knee movements.
•Consider taking lessons to learn the proper technique for sports. Have a trainer or person who is familiar with sports equipment check your equipment to see if it is well suited for your level of ability, body size, and body strength.
•If you feel that certain activities at your workplace are causing pain or soreness from overuse, call your human resources department for information on other ways of doing your job or to talk about using different equipment.
.
Tips specific to the knee
•Keep your knees and the muscles that support them strong and flexible. Warm up before activities. Try the following stretches:
?Hamstring stretch ?Knee-to-chest exercise ?Calf stretch ?Straight-leg raises •Avoid activities that stress your knees, such as deep knee bends or downhill running.
•Wear shoes with good arch supports.
•Do not wear high-heeled shoes.
•When playing contact sports, wear the right shoes that are made for the surface you are playing or running on, such as a track or tennis court.
•Replace running shoes every 300 to 500 miles (480 to 800 kilometers).
Tips specific to female athletes
Sports trainers recommend training programs that help women learn to run, jump, and pivot with knees bent to avoid knee injuries. In sports such as soccer, basketball, and volleyball, women who bend their knees and play low to the ground have fewer knee injuries than women who run and pivot with stiff legs.
Knee brace use
Some people use knee braces to prevent knee injuries or after a knee injury. There are many types of knee braces, from soft fabric sleeves to rigid, metal hinged braces, that support and protect the knee. If your doctor has recommended the use of a knee brace, follow his or her instructions. If you are using a knee brace to help prevent problems, follow the manufacturer’s instructions for use.
Keep bones strong
•Eat a nutritious diet with enough calcium and vitamin D, which helps your body absorb calcium. Calcium is found in dairy products, such as milk, cheese, and yogurt; dark green, leafy vegetables, such as broccoli; and other foods. For more information, see the topic Healthy Eating.
•Exercise and stay active. It is best to do weight-bearing exercise, such as walking, jogging, stair climbing, dancing, or lifting weights, for 45 to 60 minutes at least 4 days a week. Weight-bearing exercises stimulate new bone growth by working the muscles and bones against gravity. Exercises that are not weight-bearing, such as swimming, are good for your general health but do not stimulate new bone growth. Talk to your doctor about an exercise program that is right for you. Begin slowly, especially if you have been inactive. For more information, see the topic Fitness.
•Avoid drinking more than one alcoholic drink per day. People who drink more than this may be at higher risk for weakening bones (osteoporosis). Alcohol use also increases your risk of falling and breaking a bone.
•Stop or do not begin smoking. Smoking puts you at a much higher risk for developing osteoporosis. It also interferes with blood supply and healing. For more information, see the topic Quitting Tobacco Use.
Possible abuse
Bruises are often the first sign of abuse. Seek help if:
•You suspect abuse. Call your local child or adult protective agency, police, or a doctor, nurse, or counselor.
•You or someone you know is a victim of violence.
•You have trouble controlling your anger with a child or other person in your care. Resources are available for help.
Source: Health.com
Related articles by Zemanta
- Can You Avoid Arthritis Knee Pain by Building Thigh Muscles? (health.usnews.com)
- Relieve The Pain Of Osteoarthritis (healthadel.com)
- Women with strong thigh muscles protected from symptomatic knee osteoarthritis (scienceblog.com)
![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)