[amazon_link asins=’B01M1CO34T,B01CNGXQYU,B01C8BR84O,B01M2A8XP3,B00854L57U,B016CCG256,B01MQK1XSX,B004RR1FF6,B000HCMK90′ template=’ProductCarousel’ store=’finmeacur-20′ marketplace=’US’ link_id=’89932f47-2c8b-11e7-848e-f7afe2b071e6′]
Pain while passing urine, a desire to urinate every few minutes, an inability to pass urine despite the urge, high-coloured, cloudy urine, abdominal pain, high fever, shivering and vomiting — a few or all of these are symptoms of an infection somewhere along the urinary tract. In the elderly, the only symptom may be a change in mental status. In men, the pain may be felt in the rectal area. In children, after a period of dryness, bedwetting may recur. In babies, the temperature can fall instead of rise, and there may be jaundice. Almost 25 per cent of visits to a physician is due to this very common infection.
CLICK & SEE
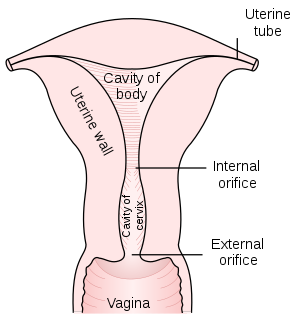
Urinary tract infection (UTI) affects all age groups and both sexes. It is much more common in women, because of the shorter urethra, its proximity to the anus, pregnancy (when the uterus obstructs the free flow of urine) and minor trauma during sexual intercourse. Thirty five per cent of women have one episode of UTI before the age of 30. Men tend to develop UTI if their prostrate gland is enlarged as this obstructs the flow of urine. In both sexes kidney stones, structural abnormalities of the urinary tract, diabetes or lack of immunity (HIV, cancer medication) can increase susceptibility to infection. Pregnant women can develop asymptomatic UTI with bacteria detected in their urine on routine examination. This condition, called “asymptomatic bactinuria” of pregnancy, needs to be treated.
...CLICK & SEE
Physicians suspect that UTI exists based on the symptoms. A routine urine examination shows abnormalities like pus cells or blood in the urine. A culture can be done to determine the organism responsible so that the appropriate antibiotic can be administered.
Untreated patients of UTI can sometimes recover spontaneously without treatment in a few months. But the infection can also enter the blood stream, causing potentially fatal septicaemia. The kidneys may become scarred, too. This leads to high blood pressure and kidney failure. During pregnancy, recurrent or chronic UTI or asymptomatic UTI compromises the placental blood supply. This affects the baby’s nutrition, leading to low birth weight and sometimes causing the mother to go into premature labour.
There are several regimens for treating UTI. Depending on the organism and antibiotic, in adult women a three-day course is usually sufficient for mild infection. In most cases and in the case of men, however, a 7-10 or 14-day course is required. Oral medication is usually sufficient. If the infection has affected the kidney, hospitalisation and intravenous medication may be required. It is important to follow the doctor’s instructions and complete the course of antibiotics even if you are symptomatically better. In women, if the symptoms do not respond and there is also white discharge, there may be an underlying pelvic infection. In men, non-responsiveness to treatment may be due to unrecognised prostatitis.
One of the ways to prevent UTI is to drink plenty of water. The urine becomes dilute and the bladder gets flushed regularly. An adult needs around 2.5 litres of water a day. In hot, humid climates and in people who exercise vigorously the requirement may go up to 4-6 litres a day. Also, drink a glass of water before going to bed. Empty the bladder before and after intercourse. Drink a glass of water after intercourse.
A few studies have shown that cranberry juice (available in India, Hindi name karaunda) and blueberry juice (not available) helps reduce the frequency and duration of UTI. This is because the juice contains vitamin C which acidifies the urine. It also contains natural chemicals that make the bladder wall slippery and prevent bacteria from sticking to it and initiating an infection. Other citrus juices and tablets of vitamin C are effective but not as efficient. A tablespoon of home-made curd taken on an empty stomach first thing in the morning naturally repopulates the intestines with “good lactobacillus”. This decreases the likelihood of the growth of disease-causing bacteria in the rectum, from where they can enter the urethra.
The pelvic muscles become lax after childbirth. This increases the possibility of the bladder and uterus descending downwards while straining. “Accidents” with leakage of urine and urgency can also occur.
All these increase the chances of infection. Keegles exercises should be done regularly soon after childbirth. Also while passing urine, consciously stop and start. This tones the pelvic muscles.
Women tend to lean forward while urinating. This position is inefficient as it increases the angle between the bladder and the urethra, creating an obstruction to the flow of urine. Women should consciously lean backwards. Also, when the area is being washed after urination or passing motion, wash from front to back. This decreases the likelihood of contamination of the urethra with rectal bacteria
Source: The Telegraph ( Kolkata, India)
Related articles
- Do I have a UTI? (zocdoc.com)
- Can cystitis result from an abortion? (zocdoc.com)
- What are the symptoms of a UTI? (zocdoc.com)
- What causes bladder infections? (zocdoc.com)
- Why does my urine hurt when I have a cold (wiki.answers.com)
- Women and Urinary Tract Infections (medtopicwriter.com)
- Probiotics Could Help Prevent Urinary Tract Infections (livescience.com)




![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)







 ..
..