[amazon_link asins=’0007169671,B005DSAMKW,B013XJPZQI,B01F2NYNF2,B015X0CQR6,B074YY8FR3,B074Z2KRNJ,B01F2O8M4Y,B071L79JQ9′ template=’ProductCarousel’ store=’finmeacur-20′ marketplace=’US’ link_id=’3e1aad7e-08f7-11e8-bbca-931ba8bdcb58′]
“Men-o-pause” may be a funny play on words but it’s no laughing matter to millions of women. When hot flashes, mood swings and memory changes are affecting your life, you want help fast. But where can you find it when the “newest” science says the old science is wrong — or even harmful?
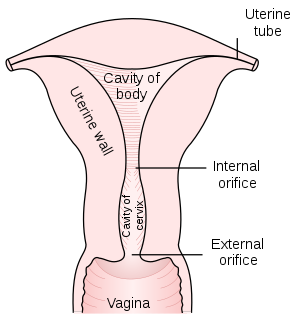
CLICK & SEE
An understanding of how and why science went astray, plus a simple, strategic plan can get your life back in balance.
What Happens During Midlife’s Pause?
Menopause is nature’s way of signaling the end of child-bearing years. When you stop having your periods naturally — usually when you’re around 50 years old — the slow-down tends to be gradual.
But menopause can occur before or after age 50, and it can also be surgically induced.
For instance, if you have your ovaries or uterus removed, you’ll skip the “peri” part and advance straight to full-blown menopause. When that happens, symptoms often intensify because there’s no gradual downshift: estrogen and progesterone production simply stops.
When menopause occurs, the primary symptoms you’re likely to experience are:
•Hot Flashes
•Vaginal Dryness
•Menstrual Irregularities (natural)
•Depression, Mood Swings
•Weight Gain (natural or surgically induced)
Short and long-term strategies can help you control these symptoms. The best approaches are preventive and involve diet and exercise. That’s not surprising because the most obvious manifestations of menopause have emerged in the last 75 years.
With a return to what’s been natural for centuries, it’s possible to minimize even the most frustrating night sweats and weight gain.
Menopause is NOT a Disease
As it is mentioned, menopause occurs when you stop producing estrogen and progesterone, and your periods cease. So, it seemed sensible to scientists that replacing those hormones would alleviate menopausal symptoms.
One of the problems with this approach was that it looked at menopause as a disease to be treated with medication, as opposed to another life stage. The other: it turned out that synthetic hormones don’t act like the real thing.
The problems will be detailed with hormone replacement later, along with information on the “new” science of bioidentical hormones.
For affordable symptom-relief right now, here are the simplest, heart-healthy ideas, followed by longer-term solutions.
Heart-Healthy, Symptom-Ease
We all hope for a quick fix. That’s not what healthy lifestyle changes are all about, but for those who want the short-list, here’s an easy way to determine if you’re in menopause, along with the “to-dos” that put you on the right track fast.
First, ask your physician for a blood test called an FSH test. It determines if your pituitary gland thinks your ovaries aren’t fully functioning, and as a result, is secreting “follicular stimulating hormone” or FSH. There is no need to do this if you have had a surgically induced menopause, as you are menopausal by definition and your FSH will be elevated.
The higher your FSH level, the more likely you’re in menopause. Peri-menopause begins the process a few years in advance; once you haven’t had a period for a year, you’re considered post-menopausal.
Just a few diet and lifestyle changes can have a dramatic effect on how you experience menopause — especially if you start making them at the “peri” stage.
Three Surefire Strategies to Start
1.Phytoestrogens. Taking Phytoestreogens or plant-estrogens before menopause can moderate day-to-day estrogen levels, so that when menopause comes, the drop won’t be so dramatic. Weak estrogens that block stronger forms, phtyoestrogens are found in licorice and alfalfa.
Royal Maca also seems to be an amazing adaptogenic herbal solution for menopause that has helped many women. Be sure to avoid the inexpensive ones, as they typically don’t work. Get the real deal from Peru.
2.Omega-3. Take high quality, animal-based omega-3 fats. A high quality animal-based omega-3 supplement, such as krill oil, can be far more effective and beneficial than fish oil. Balance omega-3 and omega-6 by eating foods rich in these oils.
3.Green tea. Polyphenols are associated with a lowered risk of heart disease, and green tea like Royal Matcha has polyphenols that can be more effective than those in red wine — plus 17 times the antioxidants of wild blueberries.
One study shows green tea can also reduce the risk of breast cancer in younger women under 50, and now, certain polyphenols have been shown to have some HRT-like benefits, without the drawbacks.
If you noticed soy isn’t on the list, it’s because non-fermented soy can damage your health.
There are also musts-to-avoid, some of which you may be aware of already. They include refined carbohydrates, sugar, caffeine and alcohol.
What to Follow Up With
Once you’ve covered the three musts to start with, add the following to your lifestage regimen:-
•Black Cohosh. It may help regulate body temperature and hot flashes.
•Locally grown, organic food
•Exercise! Start a program that you know you’ll do at least 3 times a week, even if it’s just 15 minutes a day to start.
•Vitamin D. Please review my one-hour video lecture for the latest on this essential vitamin.
The Smartest Long-Term Solutions
If you’ve developed healthy habits that support your lifestage and invested a little time exploring the web links highlighted here, work on these long-term adjustments next:
•Add low-to-moderate intensity and variety to your exercise plan
•Optimize your health with my easy Nutrition Plan
Avoid These DANGEROUS Solutions:-
It has been overwhelmingly proven that conventional hormone replacement therapy (HRT), which science once touted, is in fact, dangerous. The following prescriptions now have black box warnings and need to be avoided:
1.Premarin. Premarin is an estrogen extracted from Pregnant Mare’s Urine. We now know it is associated with an increased risk of heart disease.
2.Estrogen Therapy. Estrogen, which is extracted from Premarin, was effective in combating some menopausal symptoms but proved to have serious, negative side effects, such as the increased risk of breast cancer and an increase in insulin levels.
3.Provera. This drug is a progestin or a synthetic form of progesterone, which probably makes it even more toxic than Premarin. Its well-documented, negative side effects include blood clotting.
In addition, long-term usage studies revealed many other negative side effects of HRT, including high blood pressure and vaginal bleeding. A year after millions of women quit taking hormone replacement therapy, incidents of breast cancer fell dramatically — by 7 percent!
No wonder women now know to avoid dangerous, conventional estrogen replacement.
The “New” Science: Bioidenticals
Recently, there’s been tremendous excitement about Bioidentical Hormone Replacement Therapy (BHRT), which was even discussed on the Oprah show in a television breakthrough.
When diet and lifestyle changes are not enough, bioidentical hormones may be able to help.
However, the FDA has recently attacked BHRT, specifically estriol, effectively banning it. Ironically, the FDA is simultaneously attempting to create natural-substance knock-offs. Here’s what’s happening:
Bioidenticals, unlike synthetic hormones or natural ones from animals, are natural hormones that are bioidentical to your own.
The bioidentical that is prescribed 80 percent of the time is estriol. It’s natural, not a drug, and you get it at compounding pharmacies. The FDA is trying to require physicians who write prescriptions for it to fill out an Investigational New Drug (IND) application. It’s no simple form; it’s 40-pages long and expensive to file. And, the FDA admits it’s unaware of any adverse effects of bioidentical hormones.
The inside scoop: Estriol has been used safely for decades, and it is believed that it is particularly useful when your ovaries have been removed or you’ve had a hysterectomy. Dr. Johathan Wright, who was interviewed many times for Expert Inner Circle program, is a pioneer in bioidenticals, and you can see what he has to say about their value in this short video.
The attack on bioidenticals comes just as the FDA is advancing drugs that are synthetic knock-offs of natural estriol. Talk about an upside down world!
Note on Bioidentical Delivery Methods
As for administering bioidentical hormones, you need to know that some delivery methods are clearly superior to others.
Oral supplementation is perhaps your worst option, as your liver processes everything in your digestive tract first, before it enters your blood stream. Any method that bypasses your liver will therefore be more effective.
Hormone creams are one common alternative that achieves this. However, since progesterone is fat soluble, it can build up in your fatty tissues and lead to having too much progesterone in your body. This in turn can disrupt other hormones. It’s also near impossible to accurately determine the dose when using a cream.
Sublingual drops offer the best of both worlds, as it enters your blood stream directly and will not build up in your tissues like the cream can. It’s also much easier to determine the dose you’re taking, as each drop is about one milligram.
So you know exactly how much you’re taking. The direct delivery system also means you can oftentimes take a lower dose than you would need if you were taking it in pill form.
Knock-Off Naturals: Don’t Be Fooled
Natural estriol can’t be patented, so there are no huge profits to be made on it.
I’m not surprised its availability is being threatened. In fact fake, profit-generating versions of the real thing are mushrooming.
Omacor (an FDA-approved, Omega-3 fat fish oil), Trimesta (a knock-off of natural estriol, now Lovaza) and already FDA-approved Prestara, a pharma version of the natural hormone DHEA, will all soon be competing against what you can get cheaper. Some believe these natural knock-offs could even be dangerous.
For instance, Trimesta is taken orally, even though this is known to be a greater risk factor for endometrial cancer than taking hormones transdermally (through the skin). Prestara is taken in doses of 200 mg daily, which is too high for women — even 50 mg daily may cause women to experience undesirable side effects, including facial hair.
To support physicians’ rights to freely prescribe bioidenticals and your right to have access to them, go to the Health Freedom Foundation’s website. You’ll find updated information and a letter you can send to Congress and the President.
One Small Step Toward Lifelong Serenity
Menopause is one of those instances where what’s easiest and natural is also best. Because prevention is always the smartest medicine, start making changes in your diet and lifestyle during peri-menopause.
Sticking to the perimeter supermarket aisles, where vegetables and fruits dominate, puts you on the right path.
By the time menopause comes, you’ll have developed healthy nutritional habits that you can build on for every life stage.
Written By Dr. Mercola
References:
[1] The Mao Clinic Staff, “Menopause Symptoms,” The Mao Clinic
[2] American Physiological Society (2007, August 14). Grapes, Soy And Kudzu Blunt Some Menopausal Side Effects. ScienceDaily. Retrieved April 2, 2009
![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)