[amazon_link asins=’B003DI98D6,B000I1IWLU,B002TC8CDO,B007WZHCWK,1500124621,0982708319,B00E3X5K6Y,B01KKPKOFK’ template=’ProductCarousel’ store=’finmeacur-20′ marketplace=’US’ link_id=’c60c4f52-66c7-11e7-b339-1114d31e7483′]
[amazon_link asins=’1940561000,B005BQ4OGE,1930633203,B006LL9SH8,B00ET6B37A,1402001029,B002AQFNSG,1493942859,B005OKE91W’ template=’ProductCarousel’ store=’finmeacur-20′ marketplace=’US’ link_id=’78c43986-66c7-11e7-a83a-7d3e4182bd5f’]
Barrett’s esophagus is a condition in which the esophagus, the muscular tube that carries food and saliva from the mouth to the stomach, changes so that some of its lining is replaced by a type of tissue similar to that normally found in the intestine. This process is called intestinal metaplasia.
While Barrett’s esophagus may cause no symptoms itself, a small number of people with this condition develop a relatively rare but often deadly type of cancer of the esophagus called esophageal adenocarcinoma. Barrett’s esophagus is estimated to affect about 700,000 adults in the United States. It is associated with the very common condition gastroesophageal reflux disease or GERD.
Normal Function of the Esophagus
The esophagus seems to have only one important function in the body—to carry food, liquids, and saliva from the mouth to the stomach. The stomach then acts as a container to start digestion and pump food and liquids into the intestines in a controlled process. Food can then be properly digested over time, and nutrients can be absorbed by the intestines.
The esophagus transports food to the stomach by coordinated contractions of its muscular lining. This process is automatic and people are usually not aware of it. Many people have felt their esophagus when they swallow something too large, try to eat too quickly, or drink very hot or very cold liquids. They then feel the movement of the food or drink down the esophagus into the stomach, which may be an uncomfortable sensat
click to see the pictures..>...(01)..….(1)……..(2)..….…(3).……..(4).….
.Digestive trac
The muscular layers of the esophagus are normally pinched together at both the upper and lower ends by muscles called sphincters. When a person swallows, the sphincters relax automatically to allow food or drink to pass from the mouth into the stomach. The muscles then close rapidly to prevent the swallowed food or drink from leaking out of the stomach back into the esophagus or into the mouth. These sphincters make it possible to swallow while lying down or even upside-down. When people belch to release swallowed air or gas from carbonated beverages, the sphincters relax and small amounts of food or drink may come back up briefly; this condition is called reflux. The esophagus quickly squeezes the material back into the stomach. This amount of reflux and the reaction to it by the esophagus are considered normal.
While these functions of the esophagus are obviously an important part of everyday life, people who must have their esophagus removed, for example because of cancer, can live a relatively healthy life without it.
GERD
Having occasional liquid or gas reflux is considered normal. When it happens frequently, particularly when not trying to belch, and causes other symptoms, it is considered a medical problem or disease. However, it is not necessarily a serious one that requires seeing a physician.
The stomach produces acid and enzymes to digest food. When this mixture refluxes into the esophagus more frequently than normal, or for a longer period of time than normal, it may produce symptoms. These symptoms, often called acid reflux, are usually described by people as heartburn, indigestion, or “gas.” The symptoms typically consist of a burning sensation below and behind the lower part of the breastbone or sternum.
Almost everyone has experienced these symptoms at least once, typically after overeating. GERD symptoms can also result from being overweight, eating certain types of foods, or being pregnant. In most people, GERD symptoms last only a short time and require no treatment at all. More persistent symptoms are often quickly relieved by over-the-counter acid-reducing agents such as antacids. Common antacids are
- Alka-Seltzer
- Maalox
- Mylanta
- Pepto-Bismol
- Riopan
- Rolaids
Other drugs used to relieve GERD symptoms are antisecretory drugs such as histamine2 (H2) blockers or proton pump inhibitors. Common H2 blockers are
Common proton pump inhibitors are
- esomeprazole (Nexium)
- lansoprazole (Prevacid)
- omeprazole (Prilosec)
- pantoprazole (Protonix)
- rabeprazole (Aciphex)
People who have GERD symptoms frequently should consult a physician. Other diseases can have similar symptoms, and prescription medications in combination with other measures might be needed to reduce reflux. GERD that is untreated over a long period of time can lead to complications, such as an ulcer in the esophagus that could cause bleeding. Another common complication is scar tissue that blocks the movement of swallowed food and drink through the esophagus; this condition is called stricture.
Esophageal reflux may also cause certain less common symptoms, such as hoarseness or chronic cough, and sometimes provokes conditions such as asthma. While most patients find that lifestyle modifications and acid-blocking drugs relieve their symptoms, doctors occasionally recommend surgery. Overall, more than 60 million American adults experience GERD, making it one of the most common medical conditions.
GERD and Barrett’s Esophagus
The exact causes of Barrett’s esophagus are not known, but it is thought to be caused in part by the same factors that cause GERD. Although people who do not have heartburn can have Barrett’s esophagus, it is found about three to five times more often in people with this condition.
Barrett’s esophagus is uncommon in children. The average age at diagnosis is 60, but it is usually difficult to determine when the problem started. It is about twice as common in men as in women and much more common in white men than in men of other races.
Barrett’s esophagus does not cause symptoms itself and is important only because it seems to precede the development of a particular kind of cancer—esophageal adenocarcinoma. The risk of developing adenocarcinoma is 30 to 125 times higher in people who have Barrett’s esophagus than in people who do not. This type of cancer is increasing rapidly in white men. This increase may be related to the rise in obesity and GERD.
For people who have Barrett’s esophagus, the risk of getting cancer of the esophagus is small: less than 1 percent (0.4 percent to 0.5 percent) per year. Esophageal adenocarcinoma is often not curable, partly because the disease is frequently discovered at a late stage and because treatments are not effective.
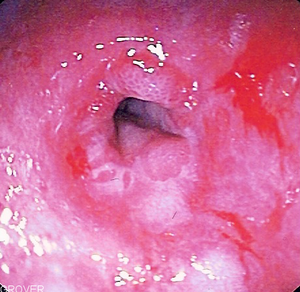
Diagnosis and ScreeningBarrett’s esophagus can only be diagnosed by an upper GI endoscopy to obtain biopsies of the esophagus. At present, it cannot be diagnosed on the basis of symptoms, physical exam, or blood tests. In an upper GI endoscopy, a flexible tube called an endoscope, which has a light and miniature camera, is passed into the esophagus. If the tissue appears suspicious, then biopsies must be done. A biopsy is the removal of a small piece of tissue using a pincher-like device passed through the endoscope. A pathologist examines the tissue under a microscope to confirm the diagnosis.
Click & see >..Normal esophagus….Metaplasia
Looking for a medical problem in people who do not know whether they have one is called screening. Currently, there are no commonly accepted guidelines on who should have endoscopy to check for Barrett’s esophagus. Among the many reasons for the lack of firm recommendations about screening are the great expense and occasional risk of side effects of the test. Also, the rate of finding Barrett’s esophagus is low, and finding the problem early has not been proven to prevent deaths from cancer.
Many physicians recommend that adult patients who are over the age of 40 and have had GERD symptoms for a number of years have endoscopy to see whether they have Barrett’s esophagus. Screening for this condition in people who have no symptoms is not recommended.
Cause and Symptoms
For unknown reasons, Barrett’s esophagus is found three times more often in males than in females. In some instances, Barrett’s esophagus appears to be congenital (present at birth). However, current evidence is strong that in most instances, it develops as a result of longstanding GERD.
Patients with Barrett’s usually have symptoms similar to those produced by chronic GERD, such as heartburn and reflux of stomach acid into the mouth. Some Barrett’s patients may also suffer from other complications of GERD, such as esophageal peptic ulcers and stricture — narrowing of the esophagus that comes from scarring. These facts are why it is important for patients with these symptoms to see their physicians regularly.
Diagnosis
Diagnosis of Barrett’s esophagus requires an examination called upper endoscopy or EGD (esophagogastroduodenoscopy). A barium x-ray is not accurate for detecting Barrett’s esophagus. An EGD is done with the patient under sedation. The physician examines the lining of the esophagus and stomach with a thin, lighted, flexible endoscope. Biopsies are performed, taking pieces of tissue to be examined under a microscope for abnormal cells which have the potential of becoming malignant. The changes may be indefinite dysplasia where the pathologist may be uncertain of the changes. In this circumstance, medical treatment is intensified and repeat biopsies are performed in 6-12 months. When dysplasia is definite, some type of definite correction is necessary.
Treatment
Barrett’s esophagus has no cure, short of surgical removal of the esophagus, which is a serious operation. Surgery is recommended only for people who have a high risk of developing cancer or who already have it. Most physicians recommend treating GERD with acid-blocking drugs, since this is sometimes associated with improvement in the extent of the Barrett’s tissue. However, this approach has not been proven to reduce the risk of cancer. Treating reflux with a surgical procedure for GERD also does not seem to cure Barrett’s esophagus.
Several different experimental approaches are under study. One attempts to see whether destroying the Barrett’s tissue by heat or other means through an endoscope can eliminate the condition. This approach, however, has potential risks and unknown effectiveness.
Surveillance for Dysplasia and Cancer
Periodic endoscopic examinations to look for early warning signs of cancer are generally recommended for people who have Barrett’s esophagus. This approach is called surveillance. When people who have Barrett’s esophagus develop cancer, the process seems to go through an intermediate stage in which cancer cells appear in the Barrett’s tissue. This condition is called dysplasia and can be seen only in biopsies with a microscope. The process is patchy and cannot be seen directly through the endoscope, so multiple biopsies must be taken. Even then, the cancer cells can be missed.
The process of change from Barrett’s to cancer seems to happen in only a few patients, less than 1 percent per year, and over a relatively long period of time. Most physicians recommend that patients with Barrett’s esophagus undergo periodic surveillance endoscopy to have biopsies. The recommended interval between endoscopies varies depending on specific circumstances, and the ideal interval has not been determined.
Treatment for Dysplasia or Esophageal Adenocarcinoma
If a person with Barrett’s esophagus is found to have dysplasia or cancer, the doctor will usually recommend surgery if the person is strong enough and has a good chance of being cured. The type of surgery may vary, but it usually involves removing most of the esophagus and pulling the stomach up into the chest to attach it to what remains of the esophagus. Many patients with Barrett’s esophagus are elderly and have many other medical problems that make surgery unwise; in these patients, other approaches to treating dysplasia are being investigated.
Things Patients Can Do
Currently, there are no medications to reverse Barrett’s esophagus. However, it appears that treating the underlying GERD may slow the progress of the disease and prevent complications. Following are some things the patient can do to help reduce acid reflux and strengthen the LES.
- Avoid eating anything within three hours before bedtime.
- Avoid smoking and tobacco products. Nicotine in the blood weakens the LES.
- Reduce consumption of fatty foods, milk, chocolate, mints, caffeine, carbonated drinks, citrus fruits and juices, tomato products, pepper seasoning, and alcohol (especially red wine).
- Eat smaller meals. Avoid tight clothing or bending over after eating.
- Review all medications with the physician. Certain drugs can actually weaken the LES.
- Elevate the head of the bed or mattress 6 to 8 inches. This helps to keep acid in the stomach. Pillows by themselves are not very helpful. Wedging pillows under the head tends to bend the body at the waist which can push more fluid back up into the esophagus.
- Lose weight if overweight. This may relieve upward pressure on the stomach and LES.
Ayurvedic Treatment
There are alternative homeopathic remedies for easing heartburn.
Alternative Treatment Of Barrett’s Esophagus , Homeopathic Treatment
Hope Through Research
Many important questions about Barrett’s esophagus need further research to
- find better ways to identify people who have the problem
- find out what causes it
- test treatments that may prevent or eliminate it
- find better treatments for people who have Barrett’s esophagus with cancer
The National Institute of Diabetes and Digestive and Kidney Diseases and the National Cancer Institute sponsor research programs to investigate Barrett’s esophagus.
Summary
Barrett’s esophagus is a condition that may develop as a result of chronic GERD. Barrett’s tissue growing in the esophagus appears to be the body’s defense against continued stomach acid irritation. Yet, this tissue does not belong in the esophagus, and for some patients, it increases the risk of developing cancer. While treatment does not reverse Barrett’s, the likelihood of developing cancer and complications can probably be reduced with a combination of diet, lifestyle changes, medication, and/or surgery. A regular program of endoscopic examination and biopsy is essential to monitor the Barrett’s tissue. By working closely with a physician, patients can expect good control of both GERD and Barrett’s, and an excellent long-term outcome.
Points to Remember
- In Barrett’s esophagus, the cells lining the esophagus change and become similar to the cells lining the intestine.
- Barrett’s esophagus is associated with gastroesophageal reflux disease or GERD.
- A small number of people with Barrett’s esophagus may develop esophageal cancer.
- Barrett’s esophagus is diagnosed by upper gastrointestinal endoscopy and biopsy.
- People who have Barrett’s esophagus should have periodic esophageal examinations.
- Taking acid-blocking drugs for GERD may result in improvements in Barrett’s esophagus.
- Removal of the esophagus is recommended only for people who have a high risk of developing cancer or who already have it.
For More Information
International Foundation for Functional Gastrointestinal Disorders (IFFGD) Inc.
P.O. Box 170864
Milwaukee, WI 53217
Phone: 1–888–964–2001 or 414–964–1799
Fax: 414–964–7176
Email: iffgd@iffgd.org
Internet:www.iffgd.org
National Cancer Institute (NCI)
National Institutes of Health
31 Center Drive
Building 31, Room 10A-19
Bethesda, MD 20892
Phone: 301–496–6641
Fax: 301–496–0846
Internet: www.nci.nih.gov
Disclaimer: This information is not meant to be a substitute for professional medical advise or help. It is always best to consult with a Physician about serious health concerns. This information is in no way intended to diagnose or prescribe remedies.This is purely for educational purpose.
Resources:
http://digestive.niddk.nih.gov/ddiseases/pubs/barretts/index.htm
http://www.gicare.com/pated/ecdgs40.htm