Alternative Names: Inflammation – esophagus
Definition:
Esophagitis is a general term for any inflammation, irritation, or swelling of the esophagus, the tube that leads from the back of the mouth to the stomach.
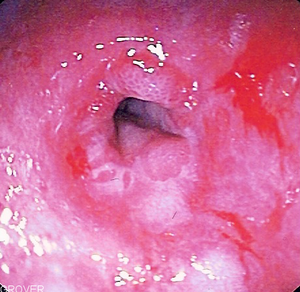
YOU MAY CLICK TO SEE THE PICTURE.……..Eosinophilic esophagitis
Esophagus is the tube that carries food from the throat to the stomach. If left untreated, this condition can become very uncomfortable, causing problems with swallowing, ulcers and scarring of the esophagus. In rare instances, a condition known as “Barrett’s esophagus” may develop, which is a risk factor for cancer of the esophagus.
Causes:
Esophagitis is frequently caused by the backflow of acid-containing fluid from the stomach to the esophagus (gastroesophageal reflux). You have a higher risk for esophagitis if you have had excessive vomiting, surgery or radiation to the chest (such as in lung cancer), or if you take medications such as aspirin, ibuprofen, potassium, alendronate, and doxycycline.
Persons with weakened immune systems due to HIV and certain medications (such as corticosteroids) may develop infections that lead to esophagitis. Esophageal infection may be due to viruses such as herpes or cytomegalovirus, and fungi or yeast (especially Candida infections).
The infection or irritation may cause the tissues to become inflamed and occasionally form ulcers. You may have difficulty when swallowing and a burning sensation in the esophagus.
Esophagitis is caused by an infection or irritation in the esophagus. An infection can be caused by bacteria, viruses, fungi or diseases that weaken the immune system. Infections that cause esophagitis include:
* Candida. This is a yeast infection of the esophagus caused by the same fungus that causes vaginal yeast infections. The infection develops in the esophagus when the body’s immune system is weak (such as in people with diabetes or HIV). It is usually very treatable with antifungal drugs.
* Herpes. Like Candida, this viral infection can develop in the esophagus when the body’s immune system is weak. It is treatable with antiviral drugs.
Irritation causing esophagitis may be caused by any of the following:
* GERD
* Vomiting
* Surgery
* Medications such as aspirin and anti-inflammatories
* Taking a large pill with too little water or just before bedtime
* Swallowing a toxic substance
* Hernias
* Radiation injury (after receiving radiation for cancer treatment)
You may click to see the related topics below:
Gastroesophageal reflux disease
Esophagitis Candida
Esophagitis CMV
Esophagitis herpes
Symptoms:
Symptoms of esophagitis include:
* Difficult and/or painful swallowing
* Heartburn (acid reflux)
* Mouth sores
* A feeling of something of being stuck in the throat
* Nausea
* Vomiting
*Oral lesions (herps)
If you have any of these symptoms, you should contact your health care provider as soon as possible.
Diagnosis:
Once your doctor has performed a thorough physical examination and reviewed your medical history, there are several tests that can be used to diagnose esophagitis. These include:
* Upper endoscopy . A test in which a long, flexible lighted tube, called an endoscope, is used to look at the esophagus.
* Biopsy. During this test, a small sample of the esophageal tissue is removed and then sent to a laboratory to be examined under a microscope.
* Upper GI series (or barium swallow). During this procedure, x-rays are taken of the esophagus after drinking a barium solution. Barium coats the lining of the esophagus and shows up white on an x-ray. This characteristic enables doctors to view certain abnormalities of the esophagus.
Treatment:
Treatment depends on the specific cause. Reflux disease may require medications to reduce acid. Infections will require antibiotics. Possible treatments include:
* Medications that block acid production, like heartburn drugs
* Antibiotics, antifungals or antivirals to treat an infection
* Pain medications that can be gargled or swallowed
* Corticosteroid medication to reduce inflammation
* Intravenous (by vein) nutrition to allow the esophagus to heal, to reduce the likelihood of malnourishment or dehydration
* Endoscopy to remove any lodged pill fragments
* Surgery to remove the damaged part of the esophagus
While being treated for esophagitis, there are certain steps you can take to help limit discomfort.
* Avoid spicy foods such as those with pepper, chili powder, curry and nutmeg.
* Avoid hard foods such as nuts, crackers and raw vegetables.
* Avoid acidic foods and beverages such as tomatoes, oranges, grapefruits and their juices. Instead, try imitation fruit drinks with vitamin C.
* Add more soft foods such as applesauce, cooked cereals, mashed potatoes, custards, puddings and high protein shakes to your diet.
* Take small bites and chew food thoroughly.
* If swallowing becomes increasingly difficult, try tilting your head upward so the food flows to the back of the throat before swallowing.
* Drink liquids through a straw to make swallowing easier.
* Avoid alcohol and tobacco.
Click for Herbal and Alternative Treatment…:->.(1).…..(2)…..(3)……(4)
You may click to learn more
Prognosis:-
The disorders that cause esophagitis usually respond to treatment.
Possible Complications :-
If untreated, esophagitis may cause severe discomfort, swallowing difficulty to the extent of causing malnutrition or dehydration, and eventual scarring of the esophagus. This scarring may lead to a stricture of the esophagus, and food or medications may not be able to pass through to the stomach.
A condition called Barrett’s esophagus can develop after years of gastroesophageal reflux. Rarely, Barrett’s esophagus may lead to cancer of the esophagus.
When to Contact a Medical Professional
Call your health care provider if you have symptoms that suggest esophagitis.
Disclaimer: This information is not meant to be a substitute for professional medical advise or help. It is always best to consult with a Physician about serious health concerns. This information is in no way intended to diagnose or prescribe remedies.This is purely for educational purpose.
Resources:
http://www.medicinenet.com/esophagitis/article.htm
http://www.nlm.nih.gov/medlineplus/ency/article/001153.htm
Related articles by Zemanta
- Drinking wine lowers risk of Barrett’s esophagus, precursor to nation’s fastest growing cancer (scienceblog.com)
- Wine May Cut Risk of Esophageal Cancer (cbsnews.com)
- Acid Reflux and Unknown Related Issues (naturalacidreflux.com)
- Treatment For Acid Reflux Does Not Improve Asthma (medicalnewstoday.com)
- Wine Consumption May Be Linked to Lower Risk of Esophageal Cancer, Studies Find (nytimes.com)
- Wine may lower risk of Barrett’s esophagus (cancercommentary.com)
- Acid Reflux Diagnosis Through Endoscopy and Biopsy (naturalacidreflux.com)












