Definition:
Ménière’s disease is a disorder of the inner ear that can affect hearing and balance to a varying degree. It is characterized by episodes of vertigo — a sensation of a spinning motion — along with fluctuating hearing loss, ringing in the ear (tinnitus), and sometimes a feeling of fullness or pressure in your ear. In most cases, Meniere’s disease affects only one ear.
CLICK TO SEE THE PICTURE
People in their 40s and 50s are more likely than people in other age groups to develop Meniere’s disease, but it can occur in anyone, even children.
click to see the picture
Although Meniere’s disease is considered a chronic condition, there are various treatment strategies that can help relieve symptoms and minimize the disease’s long-term impact on your life.
It is named after the French physician Prosper Ménière, who, in an article published in 1861, first reported that vertigo was caused by inner ear disorders. The condition affects people differently; it can range in intensity from being a mild annoyance to a chronic, lifelong disability
Symptoms:
The symptoms of Ménière’s are variable; not all sufferers experience the same symptoms. However, so-called “classic Ménière’s” is considered to have the following four symptoms:
CLICK TO SEE THE POICTURE
*Periodic episodes of rotary vertigo or dizziness.
*Fluctuating, progressive, unilateral (in one ear) or bilateral (in both ears) hearing loss, usually in lower frequencies.
*Unilateral or bilateral tinnitus.
*A sensation of fullness or pressure in one or both ears.
Ménière’s often begins with one symptom, and gradually progresses. However, not all symptoms must be present for a doctor to make a diagnosis of the disease. Several symptoms at once is more conclusive than different symptoms at separate times.
Attacks of rotational vertigo can be severe, incapacitating, and unpredictable and can last anywhere from minutes to hours, but generally no longer than 24 hours. For some sufferers however, prolonged attacks can occur, lasting from several days to several weeks, often causing the sufferer to be severely incapacitated. This combines with an increase in volume of tinnitus and temporary, albeit significant, hearing loss. Hearing may improve after an attack, but often becomes progressively worse. Nausea, vomiting, and sweating sometimes accompany vertigo, but are symptoms of vertigo, and not of Ménière’s.
Some sufferers experience what are informally known as “drop attacks”—a sudden, severe attack of dizziness or vertigo that causes the sufferer, if not seated, to fall without warning. Drop attacks are likely to occur later in the disease, but can occur at any time.[10] Patients may also experience the feeling of being pushed or pulled. Some patients may find it impossible to get up for some time, until the attack passes or medication takes effect.
In addition to hearing loss, sounds can appear tinny or distorted, and patients can experience unusual sensitivity to noises.
Some sufferers also experience nystagmus, or uncontrollable rhythmical and jerky eye movements, usually in the horizontal plane, reflecting the essential role of non-visual balance in coordinating eye movements
Migraine:
There is an increased prevalence of migraine in patients with Ménière’s disease. As well, migraine leads to a greater susceptibility of developing Ménière’s disease. The distinction between migraine-associated vertigo and Ménière’s is that migraine-associated vertigo may last for more than 24 hours
Causes:
Ménière’s disease is idiopathic, but it is believed to be linked to endolymphatic hydrops, an excess of fluid in the inner ear.
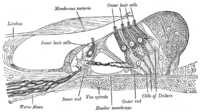
he inner ear is a cluster of connected passages and cavities called a labyrinth. The outside of the inner ear is made of bone (bony labyrinth). Inside is a soft structure of membrane (membranous labyrinth) that’s a slightly smaller, similarly shaped version of the bony labyrinth. The membranous labyrinth contains a fluid (endolymph) and is lined with hair-like sensors that respond to movement of the fluid.
 …
…
In order for all of the sensors in the inner ear to function properly, the fluid needs to retain a certain volume, pressure and chemical composition. Factors that alter the properties of inner ear fluid may help cause Meniere’s disease. Scientists have proposed a number of potential causes or triggers, including:
*Improper fluid drainage, perhaps because of a blockage or anatomic abnormality
*Abnormal immune response
*Allergies
*Viral infection
*Genetic predisposition
Because no single cause has been identified, it’s likely that Meniere’s disease is caused by a combination of factors.
Complications:
The unpredictable episodes of vertigo are usually the most debilitating problem of Meniere’s disease. The episodes often force a person to lie down for several hours and lose time from work or leisure activities, and they can cause emotional stress.
Vertigo can also increase your risk of:
*Falls
*Accidents while driving a car or operating heavy machinery
*Depression or anxiety in dealing with the disease
*Permanent hearing loss
Diagnosis:
Doctors establish a diagnosis with complaints and medical history. However, a detailed otolaryngological examination, audiometry and head MRI scan should be performed to exclude a vestibular schwannoma or superior canal dehiscence which would cause similar symptoms. There is no definitive test for Ménière’s, it is only diagnosed when all other causes have been ruled out. If any cause had been discovered, this would eliminate Ménière’s disease, as by its very definition, as an exclusively idiopathic disease, it has no known causes.
Treatment:
Because Ménière’s cannot be cured, treatments focus more on addressing symptoms. In extreme cases, it is necessary to destroy vestibular hair cells with the antibiotic streptomycin or to remove the affected labyrinth surgically in order to relieve severe vertigo. Patients are sometimes treated by the insertion of a shunt that diverts excess endolymph directly to the cerebrospinal fluid, a procedure that is not always effective. Typical remedies to improve symptoms may include:
*Antihistamines considered antiemetics such as meclozine and dimenhydrinate
*Antiemetic drugs such as trimethobenzamide.
*Antivertigo/antianxiety drugs such as betahistine and diazepam.
*Herbal remedies such as ginger root
Coping:
Sufferers tend to have high stress and anxiety due to the unpredictable nature of the disease. Healthy ways to combat this stress can include aromatherapy, yoga, T’ai chi., and meditation.
Surgery:
If symptoms do not improve with typical treatment, more permanent surgery is considered. Unfortunately, because the inner ear deals with both balance and hearing, few surgeries guarantee no hearing loss.
Nondestructive:
Nondestructive surgeries include those which do not actively remove any functionality, but rather aim to improve the way the ear works.
Intratympanic steroid treatments involve injecting steroids (commonly dexamethasone) into the middle ear in order to reduce inflammation and alter inner ear circulation.
Surgery to decompress the endolymphatic sac has shown to be effective for temporary relief from symptoms. Most patients see a decrease in vertigo occurrence, while their hearing may be unaffected. This treatment, however, does not address the long-term course of vertigo in Ménière’s disease. Danish studies even link this surgery to a very strong placebo effect, and that very little difference occurred in a 9-year followup, but could not deny the efficacy of the treatment
Destructive
Destructive surgeries are irreversible, and involve removing entire functionality of most, if not all, of the affected ear.
The inner ear itself can be surgically removed via labyrinthectomy. Hearing is always completely lost in the affected ear with this operation. Alternatively, a chemical labyrinthectomy, in which a drug (such as gentamicin) that “kills” the vestibular apparatus is injected into the middle ear can accomplish the same results while retaining hearing.
Alternatively, surgeons can cut the nerve to the balance portion of the inner ear in a vestibular neurectomy. Hearing is often mostly preserved, however the surgery involves cutting open into the lining of the brain, and a hospital stay of a few days for monitoring would be required.
Vertigo (and the associated nausea and vomiting) typically accompany the recovery from destructive surgeries as the brain learns to compensate
Physiotherapy:
Physiotherapists also have a role in the management of Meniere’s disease. In vestibular rehabilitation, physiotherapists use interventions aimed at stabilizing gaze, reducing dizziness and increasing postural balance within the context of activities of daily living. After a vestibular assessment is conducted, the physiotherapist tailors the treatment plan to the needs of that specific patient.
The central nervous system (CNS) can be re-trained because of its plasticity, or alterability, as well as its repetitious pathways. During vestibular rehabilitation, physiotherapists take advantage of this characteristic of the CNS by provoking symptoms of dizziness or unsteadiness with head movements while allowing the visual, somatosensory and vestibular systems to interpret the information. This leads to a continuous decrease in symptoms.
Although a significant amount of research has been done regarding vestibular rehabilitation in other disorders, substantially less has been done specifically on Meniere’s disease. However, vestibular physiotherapy is currently accepted as part of best practices in the management of this condition
Prognosis:
Ménière’s disease usually starts confined to one ear, but it often extends to involve both ears over time. The number of patients who end up with bilaterial Ménière’s is debated, with ranges spanning from 17% to 75%.
Some Ménière’s disease sufferers, in severe cases, may end up losing their jobs, and will be on disability until the disease burns out. However, a majority (60-80%) of sufferers will not need permanent disability and will recover with or without medical help.
Hearing loss usually fluctuates in the beginning stages and becomes more permanent in later stages, although hearing aids and cochlear implants can help remedy damage. Tinnitus can be unpredictable, but patients usually get used to it over time.
Ménière’s disease, being unpredictable, has a variable prognosis. Attacks could come more frequently and more severely, less frequently and less severely, and anywhere in between. However, Ménière’s is known to “burn out” when vestibular function has been destroyed to a stage where vertigo attacks cease.
Studies done on both right and left ear sufferers show that patients with their right ear affected tend to do significantly worse in cognitive performance. General intelligence was not hindered, and it was concluded that declining performance was related to how long the patient had been suffering from the disease
Disclaimer: This information is not meant to be a substitute for professional medical advise or help. It is always best to consult with a Physician about serious health concerns. This information is in no way intended to diagnose or prescribe remedies.This is purely for educational purpose
Resources:
http://en.wikipedia.org/wiki/M%C3%A9ni%C3%A8re’s_disease
http://www.mayoclinic.com/health/menieres-disease/DS00535
http://www.dizziness-and-balance.com/disorders/menieres/menieres.html
http://www.360balance.com/hydrops.html
Related articles
- Are You at Risk For Meniere’s Disease? (fitsugar.com)
- Defining Ménière’s Disease (everydayhealth.com)
- What is M?ni?re’s disease? (zocdoc.com)
- What is M?ni?re’s disease? (zocdoc.com)
- Labyrinthitis (findmeacure.com)
- What is the cause of Meniere’s Disease? (nuccadoctordavis.com)

![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)











