Introduction:
A kidney transplant is an operation that places a healthy kidney in your body. The transplanted kidney takes over the work of the two kidneys that failed, and you no longer need dialysis.
CLICK & SEE
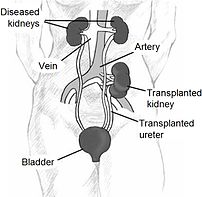
During a transplant, the surgeon places the new kidney in your lower abdomen and connects the artery and vein of the new kidney to your artery and vein. Often, the new kidney will start making urine as soon as your blood starts flowing through it. But sometimes it takes a few weeks to start working.
If you have advanced and permanent kidney failure, kidney transplantation may be the treatment option that allows you to live much like you lived before your kidneys failed. Since the 1950s, when the first kidney transplants were performed, much has been learned about how to prevent rejection and minimize the side effects of medicines.
But transplantation is not a cure; it’s an ongoing treatment that requires you to take medicines for the rest of your life. And the wait for a donated kidney can be years long.
Many transplanted kidneys come from donors who have died. Some come from a living family member. The wait for a new kidney can be long. People who have transplants must take drugs to keep their body from rejecting the new kidney for the rest of their lives.
A successful transplant takes a coordinated effort from your whole health care team, including your nephrologist, transplant surgeon, transplant coordinator, pharmacist, dietitian, and social worker. But the most important members of your health care team are you and your family. By learning about your treatment, you can work with your health care team to give yourself the best possible results, and you can lead a full, active life.
Around 40 per cent of patients with end-stage renal failure (ESRF) need a transplant which frees people from the need for dialysis treatments.
A successful kidney transplant has ten times the function of dialysis (for example ten times the ability to remove toxins and extra water from the blood). It means that transplant patients have a better quality of life, with more energy than they did on dialysis.
How transplants work:-
An assessment is necessary to determine whether your body will accept an available kidney. This may require several visits over four to six months, and all potential recipients must be healthy enough for surgery.
Although there is no age limit, few units will transplant patients over 70 years – unless very fit.
If a family member, partner or friend wants to donate a kidney, they will need to be evaluated for general health too.
If there is no potential living donor, you will need to register with hospital and be put on a national waiting list to receive a kidney from a deceased donor. but this varies considerably around the country. Kidneys can also be donated by strangers.
If there is a suitable living donor, the operation can be scheduled in advance, when it suits both sides. If you’re on a waiting list for a deceased donor kidney, as soon as it becomes available, you must go to the hospital quickly – where a test is carried out to check the kidney won’t be rejected. If it’s suitable, the transplant can proceed. The operation usually takes three to four hours.
A surgeon places the new kidney inside your lower abdomen and connects the artery and vein of the new kidney to your artery and vein. Your blood flows through the new kidney, which makes urine, just like your own kidneys did when they were healthy. Unless they are causing infection or high blood pressure, your own kidneys are left in place.
During the operation, the transplant kidney is inserted into the lower abdomen and connected to an artery and vein (to the leg). The blood flows through the new kidney, which makes urine, just like the old kidneys did when they were healthy. The old kidneys are usually left in place.
Often the new kidney will start making urine as soon as blood starts flowing through it, but about one third of patients will require dialysis for around a week. Most patients leave hospital two weeks after the operation.
To prevent the immune system from seeing the new kidney as foreign and rejecting it, you’ll have to take drugs that turn off (or suppress) your immune response (immunosupressants). It’s important to understand the instructions for taking these medicines before leaving hospital, as missing the tablets for just 24 hours can cause rejection and the loss of the kidney.
Recovery From Surgery:-
As after any major surgery, you’ll probably feel sore and groggy when you wake up. However, many transplant recipients report feeling much better immediately after surgery. Even if you wake up feeling great, you’ll need to stay in the hospital for about a week to recover from surgery, and longer if you have any complications.
Posttransplant Care:-
Your body’s immune system is designed to keep you healthy by sensing “foreign invaders,” such as bacteria, and rejecting them. But your immune system will also sense that your new kidney is foreign. To keep your body from rejecting it, you’ll have to take drugs that turn off, or suppress, your immune response. You may have to take two or more of these immunosuppressant medicines, as well as medications to treat other health problems. Your health care team will help you learn what each pill is for and when to take it. Be sure that you understand the instructions for taking your medicines before you leave the hospital.
If you’ve been on hemodialysis, you’ll find that your posttransplant diet is much less restrictive. You can drink more fluids and eat many of the fruits and vegetables you were previously told to avoid. You may even need to gain a little weight, but be careful not to gain weight too quickly and avoid salty foods that can lead to high blood pressure
Rejection:-
You can help prevent rejection by taking your medicines and following your diet, but watching for signs of rejection—like fever or soreness in the area of the new kidney or a change in the amount of urine you make—is important. Report any such changes to your health care team.
Even if you do everything you’re supposed to do, your body may still reject the new kidney and you may need to go back on dialysis. Unless your health care team determines that you’re no longer a good candidate for transplantation, you can go back on the waiting list for another kidney.
Side Effects of Immunosuppressants:
Immunosuppressants can weaken your immune system, which can lead to infections. Some drugs may also change your appearance. Your face may get fuller; you may gain weight or develop acne or facial hair. Not all patients have these problems, though, and diet and makeup can help.
Immunosuppressants work by diminishing the ability of immune cells to function. In some patients, over long periods of time, this diminished immunity can increase the risk of developing cancer. Some immunosuppressants cause cataracts, diabetes, extra stomach acid, high blood pressure, and bone disease. When used over time, these drugs may also cause liver or kidney damage in a few patients.
Hope through Research:-
The NIDDK, through its Division of Kidney, Urologic, and Hematologic Diseases, supports several programs and studies devoted to improving treatment for patients with progressive kidney disease and permanent kidney failure, including patients who receive a transplanted kidney.
•The End-Stage Renal Disease Program promotes research to reduce medical problems from bone, blood, nervous system, metabolic, gastrointestinal, cardiovascular, and endocrine abnormalities in kidney failure and to improve the effectiveness of dialysis and transplantation. The program seeks to increase kidney graft and patient survival and to maximize quality of life.
•The NIH Organ/Tissue Transplant Center, located at the NIH Clinical Center in Bethesda, MD, is a collaborative project of NIH, the Walter Reed Army Medical Center, the Naval Medical Research Center, and the Diabetes Research Institute at the University of Miami. The site includes a state-of-the-art clinical transplant ward, operating facility, and outpatient clinic designed for the study of new drugs or techniques that may improve the success of organ and tissue transplants.
•The U.S. Renal Data System (USRDS) collects, analyzes, and distributes information about the use of dialysis and transplantation to treat kidney failure in the United States. The USRDS is funded directly by NIDDK in conjunction with the Centers for Medicare & Medicaid Services. The USRDS publishes an Annual Data Report, which characterizes the total population of people being treated for kidney failure; reports on incidence, prevalence, mortality rates, and trends over time; and develops data on the effects of various treatment modalities. The report also helps identify problems and opportunities for more focused special studies of renal research issues.
Disclaimer: This information is not meant to be a substitute for professional medical advise or help. It is always best to consult with a Physician about serious health concerns. This information is in no way intended to diagnose or prescribe remedies.This is purely for educational purpose
Resources:
http://www.topnews.in/health/kidney-transplant-patients-low-physical-activity-likely-die-early-211177
http://www.nlm.nih.gov/medlineplus/kidneytransplantation.html
http://www.kidney.niddk.nih.gov/kudiseases/pubs/transplant/
http://www.bbc.co.uk/health/physical_health/conditions/in_depth/kidneys/kidneys_transplant.shtml
Related articles
- Kidney dialysis (findmeacure.com)
- Kidney Cancer (findmeacure.com)
- Can a kidney transplant get rid of kidney cancer? (zocdoc.com)
- What happens to a person after renal failure occurs? (zocdoc.com)
- Organ donations in China: Will official financial incentives starve the black market? (slate.com)
- How can I prepare for the later stages of chronic kidney disease? (zocdoc.com)
- SNPwatch: Genetic Variant Conferring Resistance to African Sleeping Sickness Linked to Kidney Transplant Function (spittoon.23andme.com)
- Why I’m Trying to Give Away a Kidney (kidneychronicles.wordpress.com)
- FAQs for Prospective Kidney Donors – Kidney Transplant – Barnes-Jewish Hospital (kidneychronicles.wordpress.com)
- Aboriginal children less likely to receive kidney transplants (eurekalert.org)
- Stem Cell Transplant Treatment for Kidney Disease (tcmremedy.wordpress.com)


![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)