[amazon_link asins=’B01A5Q746G,B01LX86E55,B00KYDCP7O,0979303605,1579548717,B01K3CXMB8,B01MRF7JRM,B01CTRKP2O,B071Y32649′ template=’ProductCarousel’ store=’finmeacur-20′ marketplace=’US’ link_id=’8f3c0421-79a1-11e7-9ce0-051296b748ee’]
Whether you are a ballerina, mountaineer, a weekend gladiator or just an office warrior, learn to protect your knees because the knee is a critical link in the kinetic chain that allows you to walk on two feet.
….....CLICK & SEE
Anit Ghosh, a former national footballer, suffered a career-threatening injury to his knee ligament five years ago. Regular and diligent post-injury rehabilitation work under the author’s guidance helped him gradually return to competitive football. Today, he turns out for Mohammedan Sporting and has learned to manage a problematic knee.
In therapy practice, over half the ladies and about one in 10 men complain of knee pain. After back pain, knee pain is the most common cause of disability and time lost from work or training.
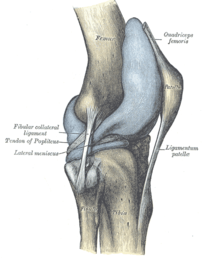
The knee is the largest joint in the human body and is formed by the articulation of three bones, the lower end of the thighbone (femur), the upper end of the shinbone (tibia) and the kneecap (patella). It may appear like a simple hinge, but besides the routine functions of bending and straightening, the knee joint performs a host of complex functions — it slides, glides, pivots, rolls and rotates — sometimes sequentially and at other times simultaneously. All these movements make the knee joint very vulnerable to shearing forces and dependant on good functional stability from the surrounding soft tissue network of ligaments, tendons and the two menisci, tough crescent-shaped cushions within the joint. In addition to the above, the knee joint also includes small, fluid-filled membranous sacs lying between the ligaments or skin, and the bones to provide smooth and frictionless gliding, like ball bearings in a machine. Furthermore, the entire articular surfaces, i.e. those that rub against one another, are covered with a tough, rubbery slippery tissue called cartilage.
Of these parts mentioned above can be a source of joint pain. Sometimes, knee pain can be caused by poor body mechanics and tight muscles elsewhere in the body and can easily be corrected by a slight alteration in gait and mechanics. For example, poor flexibility around the ankle and hip can transfer a lot of shearing forces onto the knee even though pathologically the knee is normal. The knee then is merely the “site” of the pain. The villain or “source” of pain may lie elsewhere.
The most common causes of knee pain are described below..>..CLICK & SEE
*One of the most crippling forms of knee ailment is arthritis caused by the degeneration of the cartilage coating. The cartilage has very poor blood supply and consequently nutrient supply and therefore once traumatised, has hardly any chance of healing itself. The inherent nature of the cartilage is a huge limiting factor for arthritis rehabilitation.
*Chondromalacia is the softening or the wearing away of the articular cartilage under the kneecap. The articular cartilage on the inside aspect of the kneecap comes in constant contact with the articular surfaces of the femur during normal knee motion. The knee motion can sometimes become abnormal or faulty due to muscle imbalance or biomechanical misalignment and cause the patella to rub against the femoral surfaces. Repetitive ‘rubbing’ of the surfaces causes chronic inflammation sometimes popularly known as “jumpers knee”.
*One of the most common causes of pain inside the joint is a torn meniscus. The crescent-shaped spongy tissues act as shock absorbers within the joint and when torn, either by injury or degeneration, tends to get caught in the joint, causing pain and instability.
*When the articular cartilage begins fragmenting and eroding due to extreme softening, the underlying bone gets exposed. This is a condition called osteoarthritis.
*Often traumatic injuries or contact sports mishaps cause the ligaments within the knee joint to snap. This is a very painful condition and more often than not, needs surgical correction where the surgeon has to reconstruct the ligament necessitating a long healing period.
WHAT YOU CAN DO TO MANAGE, EVEN PREVENT KNEE PAIN?
*Stretch regularly. Regular stretching of the hip flexors, hip extensors and the iliotibial band (a sheath of muscle lying on the outside of your thigh extending from the hip to the lateral aspect of the knee) will ensure good gait and running mechanics and spare the knee of shearing forces.
*Train with weights. Loading the knee and hips early in life with weights will build density in the bones and prevent erosion in later life.
*Work the hamstrings. The average person has stronger quadriceps compared to the hamstrings. Increase hamstring strength for better muscle balance and correct alignment of the kneecap. This will avoid compression forces within the knee.
*Strengthen the vastus medialis muscle — the muscles lying in the inside aspect of your front thigh. This will help to realign and track the kneecap to its normal pathway.
*Exercise discretion while performing repetitive knee motions like running, skipping, jumping etc. If you must run, learn proper running technique. Let’s face it — nine out of 10 people who visit lifestyle and recreation gyms do not have good technique. Running on the treadmill for these people is sheer disaster!
*If you are an active sort of a person, check with your doctor whether you should supplement with Glucosamine sulphate and Chondroitin. They are known to have shown results in preventing degeneration of the knee joint.
*Avoid knee extensions. The leg extension exercise is treated as a panacea for all sorts of knee ailments by trainers and therapists alike. In reality, open-chain movements like the knee extension exercise is potentially more dangerous than closed-chain movements like the lunge and squat.
*The leg extension movement causes compression between the kneecap and the thighbone and I would recommend even healthy knee-owners to stay far away from it. Choose multi-joint exercises that make the quadriceps and hamstrings work together in unison.
The best exercises for the knee are:–
*One-legged squats
*Glute ham raises
*Lunges
*Split squats
Sources: The Telegraph (Kolkata, India)
Related articles by Zemanta
- Knee Injury (findmeacure.com)
- Anterior Cruciate Ligament Injury (completerunning.com)
- Basic Knee Anatomy (blogs.webmd.com)
- Knee Pain Relief : Information About Meniscal Tears – Knee Braces That Help (articlesbase.com)
- What is a knee replacement made of? (blogs.webmd.com)
- Most Knee Pain is Caused by Arthritis (articlesbase.com)
- Knee injury likely to be treated by adult stem cell therapy (stemcell.taragana.net)
- Get The Best Knee Strengthening Exercises and More Fitness Tips (freerehabhealthinfo.vazdot.com)


![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)



