[amazon_link asins=’1591026156,B00Q08M4UA,B0112M60KI,0312990634,1541100182,1457513838,B01AJKWX2S,B015X283P8,0684814390′ template=’ProductCarousel’ store=’finmeacur-20′ marketplace=’US’ link_id=’d5c0db4e-8fe8-11e7-a343-595a702e7a5d’]
Alternative Names : Hypertrophic osteoarthritis; Osteoarthrosis; Degenerative joint disease; DJD; OA; Arthritis – osteoarthritis.
Definition : Osteoarthritis (OA) is the most common joint disorder.
Osteoarthritis (previously called degenerative arthritis, degenerative joint disease) is a chronic disorder of joint cartilage and surrounding tissues that is characterized by pain, stiffness, and loss of function.
Osteoarthritis also occurs in almost all animals with a backbone—including fish, amphibians, and birds. Because the disorder is so widespread in the animal kingdom, some authorities believe that osteoarthritis may have evolved from an ancient method of cartilage repair.
Many myths about osteoarthritis persist—for example, that it is an inevitable part of aging, like gray hair and skin changes; that it results in little disability; and that treatment is not effective. Although osteoarthritis is more common in older people, it is not caused simply by the wear and tear that occurs with years of use. Instead, microscopic changes in the structure and composition of cartilage appear to be responsible. Most people who have the disorder, especially younger people, have few if any symptoms; however, some older people develop significant disabilities.
Causes:
Most of the time, the cause of OA is unknown. It is mainly related to aging, but metabolic, genetic, chemical, and mechanical factors can also lead to OA.
Normally, joints have such a low friction level that they are protected from wearing out, even after years of use. Osteoarthritis probably begins most often with an abnormality of the cells that synthesize the components of cartilage, such as collagen (a tough, fibrous protein in connective tissue) and proteoglycans (substances that provide resilience). Next, the cartilage may swell because of water retention, become soft, and then develop cracks on the surface. Tiny cavities form in the bone beneath the cartilage, weakening the bone. Bone can overgrow at the edges of the joint, producing bumps (osteophytes) that can be seen and felt. Ultimately, the smooth, slippery surface of the cartilage becomes rough and pitted, so that the joint can no longer move smoothly and absorb impact. All the components of the joint—bone, joint capsule (tissues that enclose most joints), synovial tissue (tissue lining the joint), tendons, ligaments, and cartilage—fail in various ways, thus altering the joint.
The symptoms of osteoarthritis usually appear in middle age and almost everyone has them by age 70. Before age 55, the condition occurs equally in both sexes. However, after 55 it is more common in women.
The disease causes the cushioning (cartilage) between the bone joints to wear away, leading to pain and stiffness. As the disease gets worse, the cartilage disappears and the bone rubs on bone. Bony spurs usually form around the joint.
OA can be primary or secondary.
Primary OA occurs without any type of injury or obvious cause.
Secondary OA is osteoarthritis due to another disease or condition. The most common causes of secondary OA are metabolic conditions, such as acromegaly, problems with anatomy (for example, being bow-legged), injury, or inflammatory disorders such as septic arthritis.
Some people who repetitively stress one joint or a group of joints, such as foundry workers, coal miners, and bus drivers, are particularly at risk. Much of the risk for osteoarthritis of the knee comes from occupations that involve bending of the joint. Curiously, long-distance running champions appear not to be at higher risk of developing the disorder. However, once osteoarthritis develops, this type of exercise often makes the disorder worse. Obesity may be a major factor in the development of osteoarthritis, particularly of the knee and especially in women.
Symptoms :
The symptoms of osteoarthritis include:
*Deep aching joint pain that gets worse after exercise or putting weight on it and is relieved by rest.
*Grating of the joint with motion
*Joint pain in rainy weather
*Limited movement
Some people might not have symptoms.
Usually, symptoms develop gradually and affect only one or a few joints at first. Joints of the fingers, base of the thumbs, neck, lower back, big toes, hips, and knees are commonly affected. Pain, usually made worse by activities that involve weight bearing (such as standing), is the first symptom. In some people, the joint may be stiff after sleep or some other inactivity, but the stiffness usually subsides within 30 minutes of moving the joint.
As the condition causes more symptoms, the joint may become less movable and eventually may not be able to fully straighten or bend. The attempt of the tissues to repair may lead to new growth of cartilage, bone, and other tissue, which can enlarge the joints. The irregular cartilage surfaces cause joints to grind, grate, or crackle when they are moved. Bony growths commonly develop in the joints at the ends or middle of the fingers (called Heberden’s or Bouchard’s nodes).
Osteoarthritis
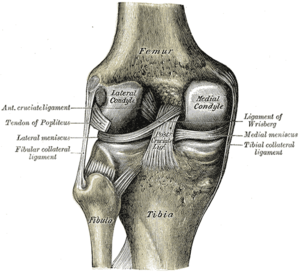
In some joints (such as the knee), the ligaments, which surround and support the joint, stretch so that the joint becomes unstable. Alternatively, the hip or knee may become stiff, losing its range of motion. Touching or moving the joint (particularly when standing, climbing stairs, or walking) can be very painful.
Osteoarthritis often affects the spine. Back pain is the most common symptom. Usually, damaged disks or joints in the spine cause only mild pain and stiffness. However, osteoarthritis in the neck or lower back can cause numbness, pain, and weakness in an arm or leg if the overgrowth of bone presses on nerves. The overgrowth of bone may be within the spinal canal, pressing on nerves before they exit the canal to go to the legs. This may cause leg pain after walking, suggesting incorrectly that the person has a reduced blood supply to the legs (intermittent claudication (see Peripheral Arterial Disease: Arteries of the Legs and Arms). Rarely, bony growths compress the esophagus, making swallowing difficult.
Osteoarthritis may be stable for many years or may progress very rapidly, but most often it progresses slowly after symptoms develop. Many people develop some degree of disability.
Diagnosis:
Exams and Tests
A physical exam can show limited range of motion, grating of a joint with motion, joint swelling, and tenderness.
An x-ray of affected joints will show loss of the joint space, and in advanced cases, wearing down of the ends of the bone and bone spurs.
The doctor makes the diagnosis based on the characteristic symptoms, physical examination, and the x-ray appearance of joints (such as bone enlargement and narrowing of the joint space). By age 40, many people have some evidence of osteoarthritis on x-rays, especially in weight-bearing joints such as the hip and knee, but only half of these people have symptoms. However, x-rays are not very useful for detecting osteoarthritis early because they do not show changes in cartilage, which is where the earliest abnormalities occur. Also, changes on the x-ray correlate poorly with symptoms. For example, an x-ray may show only a minor change while the person is having severe symptoms, or an x-ray may show numerous changes while the person is having very few, if any, symptoms.
Magnetic resonance imaging (MRI) can reveal early changes in cartilage, but it is rarely needed for the diagnosis. Also, MRI is too expensive to justify routine use. There are no blood tests for the diagnosis of osteoarthritis, although blood tests may help rule out other disorders
Treatment :
The goals of treatment are to relieve pain, maintain or improve joint movement, increase the strength of the joints, and reduce the disabling affects of the disease. The treatment depends on which joints are involved.
MEDICATIONS:
The most common medications used to treat osteoarthritis are nonsteroidal anti-inflammatory drugs (NSAIDs). They are pain relievers that reduce pain and swelling. Types include aspirin, ibuprofen, and naproxen.
Although NSAIDs work well, long-term use of these drugs can cause stomach problems, such as ulcers and bleeding. Manufacturers of NSAIDs include a warning label on their products that alerts users to an increased risk for cardiovascular events (heart attacks and strokes) and gastrointestinal bleeding.
Other medications used to treat OA include:
- COX-2 inhibitors (coxibs). Coxibs block a substance called COX-2 that causes swelling. This class of drugs was first thought to work as well as other NSAIDs, but with fewer stomach problems. However, reports of heart attacks and stroke have led the FDA to re-evaluate the risks and benefits of the COX-2s. Celecoxib (Celebrex) is still available at the time of this report, but labeled with strong warnings and a recommendation that it be prescribed at the lowest possible dose for the shortest possible period of time. Ask your doctor whether the drug is right and safe for you.
- Steroids. These medications are injected right into the joint. They can also be used to reduce inflammation and pain.
- Supplements. Many people are helped by over-the-counter remedies such as glucosamine and chondroitin sulfate. There is some evidence that these supplements can help control pain, although they do not seem to grow new cartilage.
- Artificial joint fluid (Synvisc, Hyalgan). These medications can be injected into the knee. They may relieve pain for up to 6 months.
LIFESTYLE CHANGES
Exercise helps maintain joint and overall movement. Ask your health care provider to recommend an appropriate home exercise routine. Water exercises, such as swimming, are especially helpful.
Applying heat and cold, protecting the joints, using self-help devices, and rest are all recommended.
Good nutrition and careful weight control are also important. If you’re overweight, losing weight will reduce the strain on the knee and ankle joints.
PHYSICAL THERAPY
Physical therapy can help improve muscle strength and the motion at stiff joints. Therapists have many techniques for treating osteoarthritis. If therapy does not make you feel better after 3-6 weeks, then it likely will not work at all.
BRACES
Splints and braces can sometimes support weakened joints. Some prevent the joint from moving; others allow some movement. You should use a brace only when your doctor or therapist recommends one. Using a brace the wrong way can cause joint damage, stiffness, and pain.
SURGERY
Severe cases of osteoarthritis might need surgery to replace or repair damaged joints. Surgical options include:
- Total or partial replacement of the damaged joint with an artificial joint (knee arthroplasty,hip arthroplasty)
- Arthroscopic surgery to trim torn and damaged cartilage and wash out the joint
- Cartilage restoration to replace the damaged or missing cartilage in some younger patents with arthritis
- Change in the alignment of a bone to relieve stress on the bone or joint (osteotomy)
- Surgical fusion of bones, usually in the spine (arthrodesis)
Prognosis:
Your movement may become very limited. Treatment generally improves function.
Possible Complications :
Decreased ability to walk
Decreased ability to perform everyday activities, such as personal hygiene, household chores, or cooking
Adverse reactions to drugs used for treatment
Surgical complications
When to Contact a Medical Professional
Complementary or alternative therapies for osteoarthritis
Use of Alternative Therapy, Quality of Life, And Healthcare Spending in Chinese Patients with Osteoarthritis.
Acupuncture Therapy , methods
Call your health care provider if you have symptoms of osteoarthritis.
Prevention :
Weight loss can reduce the risk of knee osteoarthritis in overweight women.
How to Live With Osteoarthritis :
*Exercise affected joints gently (in a pool, if possible)
*Massage at and around affected joints (this measure should preferably be performed by a trained therapist)
*Apply a heating pad or a damp and warm towel to affected joints
*Maintain an appropriate weight (so as not to place extra stress on joints)
*Use special equipment as necessary (for example, cane, crutches, walker, neck collar, or elastic knee support to protect joints from overuse; a fixed seat placed in a bathtub to enable less stretching while washing)
*Wear well-supported shoes or athletic shoes
Disclaimer: This information is not meant to be a substitute for professional medical advise or help. It is always best to consult with a Physician about serious health concerns. This information is in no way intended to diagnose or prescribe remedies.This is purely for educational purpose
Resources:
http://www.nlm.nih.gov/medlineplus/ency/article/000423.htm
http://www.merck.com/mmhe/sec05/ch066/ch066a.html






























![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)