Introduction:
In order for blood to perform its essential functions of bringing nutrients and oxygen to the cells of the body, and carrying waste materials away from those cells, the chemical composition of the blood must be carefully controlled. Blood contains particles of many different sizes and types, including cells, proteins, dissolved ions, and organic waste products. Some of these particles, such as proteins like hemoglobin, are essential for the body. Others, such as urea (a waste product from protein metabolism), must be removed from the blood or they will accumulate and interfere with normal metabolic processes. Still other particles, including many of the simple ions dissolved in the blood, are required by the body in certain concentrations that must be tightly regulated, especially when the intake of these chemicals varies. The body has many different means of controlling the chemical composition of the blood. For instance, you learned in the “Iron Use and Storage in the Body: Ferritin and Molecular Representations” tutorial that the ferritin protein can help to control the amount of free iron in the blood. As you will discover in the tutorial entitled, “Blood, Sweat, and Buffers: pH Regulation During Exercise”, buffers dissolved in the blood can help regulate the blood’s pH. But the largest responsibility for maintaining the chemistry of the blood falls to the kidneys, a pair of organs located just behind the lining of the abdominal cavity. It is the job of the kidneys to remove the harmful particles from the blood and to regulate the blood’s ionic concentrations, while keeping the essential particles in the blood
CLICK & SEE THE PICTURES
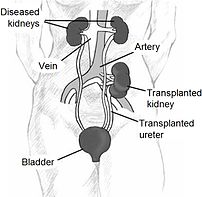
Healthy kidneys clean the blood by removing excess fluid, salt and wastes. When they fail, harmful wastes build up, blood pressure may rise, and the body may retain excess fluid. When this happens, treatment – dialysis or a kidney transplant – is needed to replace the work of the failed kidneys, which is known as end-stage renal failure (ESRF).
There are three primary and two secondary types of dialysis: hemodialysis (primary), peritoneal dialysis (primary), hemofiltration (primary), hemodiafiltration (secondary), and intestinal dialysis (secondary).
Hemodialysis:
Haemodialysis (HD) is the most common method used to treat ESRF and has been available since the 1960s. Despite some advances in dialysis machines in recent years, HD is still a complicated and inconvenient therapy requiring a coordinated effort from a large healthcare team, including:
•GP
•Nephrologist (kidney doctor)
•Dialysis nurse
•Dialysis technician
•Dietitian
•Social worker
One important step before starting HD is a small operation to prepare a site on the body. One of the arteries in your arm is re-routed to join a vein, forming a fistula. Blood is removed from the fistula, cleaned and returned to it, allowing dialysis process to take place.
Needles are inserted into a fistula (the point of access to the bloodstream) at the start of HD. You may find this one of the hardest parts, although most people report getting used to them after a few sessions. If it’s painful, an anesthetic cream or spray can be applied to the skin.
In HD, blood is allowed to flow, a small amount at a time, through a special filter (the ‘dialyser’ or ‘artificial kidney’) that removes wastes and extra fluids. The clean blood is then returned to your body via the fistula. This helps to keep the correct amount of water in the body, control blood pressure – and keep the proper balance of chemicals such as potassium, sodium and acid.
Most people have HD three times a week for three to five hours, with a morning, afternoon or evening ‘slot’; depending on availability and capacity at a dialysis unit, usually in a large hospital. Some receive it at a smaller satellite unit nearer home, and a few have HD in their own homes.
By learning about the treatment, and working with your healthcare team, it’s possible to have a full, active life
Peritoneal dialysis:
Peritoneal dialysis (PD) became an alternative to HD in the 1980s, with many preferring the independence it brings them.
It means you don’t have to have dialysis sessions at a unit, but can give treatments at home, at work or on holiday. Like HD, by learning about the treatment, and working with the medical team, it’s possible to have a full and active life.
In PD, a soft tube called a catheter is used to fill the abdomen with a cleansing liquid called dialysis solution. The abdominal cavity is lined with a layer called the peritoneum. Waste products and extra fluid (and salt) then pass through the peritoneum from the blood into the dialysis solution. They then leave the body when the dialysis solution is drained. This used solution is then thrown away.
The process of draining and filling is called an ‘exchange’ and takes about 30 to 40 minutes. The period the dialysis solution is in the abdomen is called the ‘dwell time’. A typical schedule is four exchanges a day, each with a dwell time of four to eight hours.
There are many forms of PD. One doesn’t even require a machine and it’s possible to walk around with the dialysis solution in your abdomen. Talk to your specialist about what’s best for your particular situation.
Whatever form is chosen, an operation is needed to have the soft catheter placed in the abdomen, which will carry the dialysis solution in and out of the abdomen. It’s usually inserted two weeks before dialysis proceeds, to allow scar tissue to build up that will hold it in place.
Hemofiltration:
Hemofiltration is a similar treatment to hemodialysis, but it makes use of a different principle. The blood is pumped through a dialyzer or “hemofilter” as in dialysis, but no dialysate is used. A pressure gradient is applied; as a result, water moves across the very permeable membrane rapidly, “dragging” along with it many dissolved substances, importantly ones with large molecular weights, which are cleared less well by hemodialysis. Salts and water lost from the blood during this process are replaced with a “substitution fluid” that is infused into the extracorporeal circuit during the treatment. Hemodiafiltration is a term used to describe several methods of combining hemodialysis and hemofiltration in one process.
Hemodiafiltration:
Hemodialfiltration is a combination of hemodialysis and hemofiltration. In theory, this technique offers the advantages of both hemodialysis and hemofiltration.
Intestinal dialysis:
In intestinal dialysis, the diet is supplemented with soluble fibres such as acacia fibre, which is digested by bacteria in the colon. This bacterial growth increases the amount of nitrogen that is eliminated in fecal waste. An alternative approach utilizes the ingestion of 1 to 1.5 liters of non-absorbable solutions of polyethylene glycol or mannitol every fourth hour.
Which is better?
Neither technique ‘cures’ ESRF, as they only provide about five per cent of normal kidney function. In other words, they control kidney failure to an extent. It’s hard to state which technique is ‘better’ for which patient, as both have pros and cons. Many patients will have both in their continuing treatment.
Living with dialysis
Adjusting to the effects of ESRF and the time spent on dialysis can be difficult. Aside from the ‘lost time’ (dialysis can take six to eight hours a day) most patients feel they have less energy. Many need to make changes in their work or home life, and can feel depressed when starting the process, or after several months of treatment. It’s good to talk with a social worker, nurse or doctor as this is a common problem that can often be treated effectively.
If you’re feeling well, your kidney specialist should measure the effectiveness of the dialysis with blood tests at least once a month in HD, and once every three months in PD.
Disclaimer: This information is not meant to be a substitute for professional medical advise or help. It is always best to consult with a Physician about serious health concerns. This information is in no way intended to diagnose or prescribe remedies.This is purely for educational purpose
Resources:
http://www.bbc.co.uk/health/physical_health/conditions/in_depth/kidneys/kidneys_dialysis.shtml
http://en.wikipedia.org/wiki/Dialysis
http://www.chemistry.wustl.edu/~edudev/LabTutorials/Dialysis/Kidneys.html
Related articles
- Can dialysis result in a lack of appetite? (zocdoc.com)
- How will my dialysis treatments affect my daily activities? (zocdoc.com)
- What is a nephrectomy? (zocdoc.com)
- Higher Death Rates Seen in Central Line Dialysis Patients (nlm.nih.gov)
- How long can a person survive on dialysis? (zocdoc.com)
- Kidney disease coupled with heart disease common problem in elderly (eurekalert.org)
- Hemodialysis vascular access modifies the association between dialysis modality and survival (medicalxpress.com)
- Meal Plans for Dialysis Patients (brighthub.com)
- Kidney dialysis myths and answers (kevinmd.com)


![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)