[amazon_link asins=’B010WHYAI8,B000OI0GZC,B00G6AB71Y,B016HW4KMS,B072F1XDPG,B01BQA2DLQ’ template=’ProductCarousel’ store=’finmeacur-20′ marketplace=’US’ link_id=’7256bb3f-c696-11e7-a513-3108b805401d’]
Definition:
Amniocentesis (also referred to as amniotic fluid test or AFT), is a medical procedure used in prenatal diagnosis of chromosomal abnormalities and fetal infections, in which a small amount of amniotic fluid, which contains fetal tissues, is extracted from the amnion or amniotic sac surrounding a developing fetus, and the fetal DNA is examined for genetic abnormalities
Tests of fetal cells found in this fluid can reveal the presence of Down syndrome or other chromosome problems in the baby. Amniocentesis can also show whether the lungs of the baby are mature enough to allow it to survive if it were elivered right away.
Amniocentesis is often recommended for pregnant women over age 35, women who have an abnormal “triple screen” blood test during pregnancy, or women who have (or whose husbands have) a family history of certain diseases or birth defects.
How do you prepare for the test?
You should have a serious discussion with your obstetrician regarding whether to have amniocentesis. Amniocentesis may be done anytime between the 14th and 20th weeks of pregnancy to test for fetal abnormalities. To check on fetal lung development, the test may be done late in the third trimester.
Tell your doctor ahead of time if you have ever had an allergic reaction to lidocaine or the numbing medicine used at the dentist’s office.
Just before the test, you should empty your bladder.
How the test is performed ?
Before the actual procedure, a local anesthetic is sometimes given to relieve the pain when inserting the needle used to withdraw the fluid. A needle is usually inserted through the mother’s abdominal wall through the wall of the uterus into the amniotic sac. With the aid of ultrasound-guidance, a physician aims towards an area of the sac that is away from the fetus and extracts approximately 20ml of amniotic fluid for testing. The puncture heals, and the amniotic sac replenishes the liquid over a day or so. After the amniotic fluid is extracted, the fetal cells are separated from it. The cells are grown in a culture medium, then fixed and stained. Under a microscope the chromosomes are examined for abnormalities. The most common abnormalities detected are Down syndrome, Edward syndrome [Trisomy 18] and Turner syndrome [Monosomy X]. Amniocentesis is most safely performed after the 14th-16th week of pregnancy, does not need to be done before then due to risk it can to to the babys limbs. Usually genetic counseling is offered prior to amniocentesis.
What happens when the test is performed?
You wear a hospital gown and lie on your back on a table. An ultrasound is done to show the location of the fetus and placenta. Your lower abdomen is cleaned with an antibacterial soap. In some cases, the doctor uses a small needle to inject a numbing medicine just under the skin, so you do not feel the amniocentesis sampling needle later. (Because the sampling needle does not cause much more stinging than the numbing medicine itself, not every doctor includes this step.)
The hollow sampling needle is several inches long and is inserted through the skin and abdominal muscle and then through the wall of the uterus. A syringe attached to the needle is used to collect a sample of fluid.
The baby’s heart tones and the mother’s blood pressure and heart rate are checked at the beginning and end of the procedure. The whole procedure takes close to 30 minutes.
Risk Factors:
Although the procedure is routine, possible complications include infection of the amniotic sac from the needle, and failure of the puncture to heal properly, which can result in leakage or infection. Serious complications can result in miscarriage. Other possible complications include preterm labor and delivery, respiratory distress, postural deformities, fetal trauma and alloimmunisation (rhesus disease). Studies from the 1970s originally estimated the risk of amniocentesis-related miscarriage at around 1 in 200 (0.5%). A more recent study (2006) has indicated this may actually be much lower, perhaps as low as 1 in 1,600 (0.06%). In contrast, the risk of miscarriage from chorionic villus sampling (CVS) is believed to be approximately 1 in 100, although CVS may be done up to four weeks earlier, and may be preferable if the possibility of genetic defects is thought to be higher
Most women experience a few hours of mild pelvic cramping, and a few will have slight vaginal bleeding. About 1 in 100 women will have a temporary leak of amniotic fluid through the vagina; this usually causes no problem.
There is a small risk of miscarriage associated with amniocentesis; this occurs in about 1 in every 200 to 400 cases, depending in part on the timing of the test and the experience level of the physician performing it. Other risks (such as infection or injury to the fetus that does not cause miscarriage) are extremely rare.
What must you do after the test is over?
If the test confirms that you are Rh incompatible with the fetus, you will need to receive an injection of a medicine called Rh immune globulin (Rhogam) to protect the baby from complications.
Let your doctor know immediately if you are having any vaginal bleeding, fluid leakage, or strong abdominal pain.
Time to know the result:
Chromosome analysis of the fluid sample takes two weeks or more. The results of some tests may be available sooner.
Amniocentesis and stem cells:
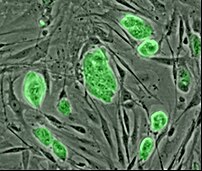
Recent studies discovered that in amniotic fluid there are a lot of multipotent stem cell, mesenchymal, hematopoietic, neural,epithelial and endothelial stem cell[1][2][3]. Amniotic stem cells don’t have ethical problem. In fact, in harvesting embryonic stem cells, a human embryo is destroyed, and so it’s considered it immoral. Another potential benefit of using amniotic stem cells over those obtained from embryos is that they side-step ethical concerns among pro-life activists by obtaining pluripotent lines of undifferentiated cells without harm to a fetus or destruction of an embryo.
Artificial heart valves, working tracheas, as well as muscle, fat, bone, heart, neural and liver cells have all been engineered through use of amniotic stem cells [4]. Tissues obtained from amniotic cell lines show enormous promise for patients suffering from congenital diseases/malformations of the heart, liver, lungs, kidneys, and cerebral tissue
You may click to see:->HOW TO – Isolate amniotic stem cells from a placenta, at home
Resources:
https://www.health.harvard.edu/fhg/diagnostics/amniosentesis.shtml
http://en.wikipedia.org/wiki/Amniocentesis
http://healthlibrary.epnet.com/GetContent.aspx?token=7e9094f4-c284-4b3a-8f7c-867fd12b36ee&chunkiid=14762
Related articles by Zemanta
- Stem cell limits set to be lifted (msnbc.msn.com)
- Amniotic Fluid May Provide New Source Of Stem Cells For Future Therapies (medicalnewstoday.com)
- Amniotic fluid may provide new source of stem cells for future therapies (scienceblog.com)
- What Is Down Syndrome? What Causes Down Syndrome? (medicalnewstoday.com)
- Week 34 of Pregnancy (mypregnancysymptoms.blogspot.com)





![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)