Definition:
Leukemia or leukaemia (Greek leukos “white”; aima “blood”) is a cancer of the blood or bone marrow and is characterized by an abnormal proliferation (production by multiplication) of blood cells, usually white blood cells (leukocytes). Leukemia is a broad term covering a spectrum of diseases. In turn, it is part of the even broader group of diseases called hematological neoplasms.
Leukemia is a type of cancer. Cancer is a group of many related diseases. All cancers begin in cells, which make up blood and other tissues. Normally, cells grow and divide to form new cells as the body needs them. When cells grow old, they die, and new cells take their place.
CLICK & SEE THE PICTURES
Sometimes this orderly process goes wrong. New cells form when the body does not need them, and old cells do not die when they should. Leukemia is cancer that begins in blood cells.
Leukemia is a malignant cancer of the blood and bone marrow that affects thousands of children and adults. Acute leukemia progresses quickly while chronic leukemia develops more slowly.
The immune system protects the body from potentially harmful substances. The inflammatory response (inflammation) is part of innate immunity. It occurs when tissues are injured by bacteria, trauma, toxins, heat or any other cause.
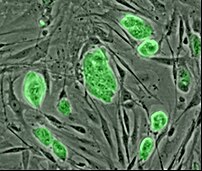
Normal blood cells
Blood cells form in the bone marrow. Bone marrow is the soft material in the center of most bones.
Immature blood cells are called stem cells and blasts. Most blood cells mature in the bone marrow and then move into the blood vessels. Blood that flows through the blood vessels and heart is called the peripheral blood.
The bone marrow makes different types of blood cells. Each type has a special function:
CLICK & SEE
White Blood Cell…..Red Blood Cell……. Platelets for blood cloting…………..Leukemia
Leukemia cells:-
In people with leukemia, the bone marrow produces abnormal white blood cells. The abnormal cells are leukemia cells. At first, leukemia cells function almost normally. In time, they may crowd out normal white blood cells, red blood cells, and platelets. This makes it hard for blood to do its work.
Types Of Leukemia:-
The types of leukemia are grouped by how quickly the disease develops and gets worse. Leukemia is either chronic (gets worse slowly) or acute (gets worse quickly):
Chronic leukemia—Early in the disease, the abnormal blood cells can still do their work, and people with chronic leukemia may not have any symptoms. Slowly, chronic leukemia gets worse. It causes symptoms as the number of leukemia cells in the blood rises.
Acute leukemia—The blood cells are very abnormal. They cannot carry out their normal work. The number of abnormal cells increases rapidly. Acute leukemia worsens quickly.
The types of leukemia are also grouped by the type of white blood cell that is affected. Leukemia can arise in lymphoid cells or myeloid cells. Leukemia that affects lymphoid cells is called lymphocytic leukemia. Leukemia that affects myeloid cells is called myeloid leukemia or myelogenous leukemia.
There are four common types of leukemia:
1.Chronic lymphocytic leukemia (chronic lymphoblastic leukemia, CLL) accounts for about 7,000 new cases of leukemia each year. Most often, people diagnosed with the disease are over age 55. It almost never affects children.
2.Chronic myeloid leukemia (chronic myelogenous leukemia, CML) accounts for about 4,400 new cases of leukemia each year. It affects mainly adults.
3.Acute lymphocytic leukemia (acute lymphoblastic leukemia, ALL) accounts for about 3,800 new cases of leukemia each year. It is the most common type of leukemia in young children. It also affects adults.
4.Acute myeloid leukemia (acute myelogenous leukemia, AML) accounts for about 10,600 new cases of leukemia each year. It occurs in both adults and children.
Hairy cell leukemia is a rare type of chronic leukemia. This booklet does not deal with hairy cell leukemia or other rare types of leukemia. Together, these rare leukemias account for about 5,200 new cases of leukemia each year. The Cancer Information Service (1-800-4-CANCER) can provide information about these types of leukemia.
Causes:
No one knows the exact causes of leukemia. Doctors can seldom explain why one person gets this disease and another does not. However, research has shown that people with certain risk factors are more likely than others to develop leukemia. A risk factor is anything that increases a person’s chance of developing a disease.
Studies have found the following risk factors for leukemia:
Very high levels of radiation —People exposed to very high levels of radiation are much more likely than others to develop leukemia. Very high levels of radiation have been caused by atomic bomb explosions (such as those in Japan during World War II) and nuclear power plant accidents (such as the Chernobyl [also called Chornobyl] accident in 1986).
Medical treatment that uses radiation can be another source of high-level exposure. Radiation used for diagnosis, however, exposes people to much lower levels of radiation and is not linked to leukemia.
Working with certain chemicals—Exposure to high levels of benzene in the workplace can cause leukemia. Benzene is used widely in the chemical industry. Formaldehyde is also used by the chemical industry. Workers exposed to formaldehyde also may be at greater risk of leukemia.
*Chemotherapy—Cancer patients treated with certain cancer-fighting drugs sometimes later develop leukemia. For example, drugs known as alkylating agents are associated with the development of leukemia many years later.
*Down syndrome and certain other genetic diseases—Some diseases caused by abnormal chromosomes may increase the risk of leukemia.
*Human T-cell leukemia virus-I (HTLV-I)—This virus causes a rare type of chronic lymphocytic leukemia known as human T-cell leukemia. However, leukemia does not appear to be contagious.
*Myelodysplastic syndrome—People with this blood disease are at increased risk of developing acute myeloid leukemia.
Symptoms:-
Like all blood cells, leukemia cells travel through the body. Depending on the number of abnormal cells and where these cells collect, patients with leukemia may have a number of symptoms.
Common symptoms of leukemia:
*Fevers or night sweats
*Frequent infections
*Feeling weak or tired
*Headache
*Bleeding and bruising easily (bleeding gums, purplish patches in the skin, or tiny red spots under the skin)
*Pain in the bones or joints
*Swelling or discomfort in the abdomen (from an enlarged spleen)
*Swollen lymph nodes, especially in the neck or armpit
*Weight loss
Such symptoms are not sure signs of leukemia. An infection or another problem also could cause these symptoms. Anyone with these symptoms should see a doctor as soon as possible. Only a doctor can diagnose and treat the problem.
In the early stages of chronic leukemia, the leukemia cells function almost normally. Symptoms may not appear for a long time. Doctors often find chronic leukemia during a routine checkup—before there are any symptoms. When symptoms do appear, they generally are mild at first and get worse gradually.
In acute leukemia, symptoms appear and get worse quickly. People with this disease go to their doctor because they feel sick. Other symptoms of acute leukemia are vomiting, confusion, loss of muscle control, and seizures. Leukemia cells also can collect in the testicles and cause swelling. Also, some patients develop sores in the eyes or on the skin. Leukemia also can affect the digestive tract, kidneys, lungs, or other parts of the body.
Click to see :->Tips to know the symptoms of Leukemia
Diagnisis:
If a person has symptoms that suggest leukemia, the doctor may do a physical exam and ask about the patient’s personal and family medical history. The doctor also may order laboratory tests, especially blood tests.
The exams and tests may include the following:
*Physical exam—The doctor checks for swelling of the lymph nodes, spleen, and liver.
*Blood tests—The lab checks the level of blood cells. Leukemia causes a very high level of white blood cells. It also causes low levels of platelets and hemoglobin, which is found inside red blood cells. The lab also may check the blood for signs that leukemia has affected the liver and kidneys.
*Biopsy—The doctor removes some bone marrow from the hipbone or another large bone. A pathologist examines the sample under a microscope. The removal of tissue to look for cancer cells is called a biopsy. A biopsy is the only sure way to know whether leukemia cells are in the bone marrow.
There are two ways the doctor can obtain bone marrow. Some patients will have both procedures:
*Bone marrow aspiration: The doctor uses a needle to remove samples of bone marrow.
*Bone marrow biopsy: The doctor uses a very thick needle to remove a small piece of bone and bone marrow.
Local anesthesia helps to make the patient more comfortable.
*Cytogenetics—The lab looks at the chromosomes of cells from samples of peripheral blood, bone marrow, or lymph nodes.
*Spinal tap—The doctor removes some of the cerebrospinal fluid (the fluid that fills the spaces in and around the brain and spinal cord). The doctor uses a long, thin needle to remove fluid from the spinal column. The procedure takes about 30 minutes and is performed with local anesthesia. The patient must lie flat for several hours afterward to keep from getting a headache. The lab checks the fluid for leukemia cells or other signs of problems.
Chest x-ray—The x-ray can reveal signs of disease in the chest.
A person who needs a bone marrow aspiration or bone marrow biopsy may want to ask the doctor the following questions:-
*Will you remove the sample of bone marrow from the hip or from another bone?
*How long will the procedure take? Will I be awake? Will it hurt?
*How soon will you have the results? Who will explain them to me?
*If I do have leukemia, who will talk to me about treatment? When?
Treatment:-
Many people with leukemia want to take an active part in making decisions about their medical care. They want to learn all they can about their disease and their treatment choices. However, the shock and stress after a diagnosis of cancer can make it hard to think of everything to ask the doctor. Often it helps to make a list of questions before an appointment. To help remember what the doctor says, patients may take notes or ask whether they may use a tape recorder. Some also want to have a family member or friend with them when they talk to the doctor—to take part in the discussion, to take notes, or just to listen.
The doctor may refer patients to doctors who specialize in treating leukemia, or patients may ask for a referral. Specialists who treat leukemia include hematologists, medical oncologists, and radiation oncologists. Pediatric oncologists and hematologists treat childhood leukemia.
Whenever possible, patients should be treated at a medical center that has doctors experienced in treating leukemia. If this is not possible, the patient’s doctor may discuss the treatment plan with a specialist at such a center.
Getting a second opinion
Sometimes it is helpful to have a second opinion about the diagnosis and the treatment plan. Some insurance companies require a second opinion; others may cover a second opinion if the patient or doctor requests it. There are a number of ways to find a doctor for a second opinion:
The patient’s doctor may be able to suggest a doctor who specializes in adult or childhood leukemia. At cancer centers, several specialists often work together as a team.
The Cancer Information Service, at 1-800-4-CANCER, can tell callers about nearby treatment centers.
A local or state medical society, a nearby hospital, or a medical school can usually provide the names of specialists.
The American Board of Medical Specialties (ABMS) has a list of doctors who have met certain education and training requirements and have passed specialty examinations. The Official ABMS Directory of Board Certified Medical Specialists lists doctors’ names along with their specialty and their educational background. The directory is available in most public libraries. Also, ABMS offers this information on the Internet .
Preparing for treatment
The doctor can describe treatment choices and discuss the results expected with each treatment option. The doctor and patient can work together to develop a treatment plan that fits the patient’s needs.
Treatment depends on a number of factors, including the type of leukemia, the patient’s age, whether leukemia cells are present in the cerebrospinal fluid, and whether the leukemia has been treated before. It also may depend on certain features of the leukemia cells. The doctor also takes into consideration the patient’s symptoms and general health.
These are some questions a person may want to ask the doctor before treatment begins:
*What type of leukemia do I have?
*What are my treatment choices? Which do you recommend for me? Why?
*What are the benefits of each kind of treatment?
*What are the risks and possible side effects of each treatment?
*If I have pain, how will you help me?
*What is the treatment likely to cost?
*How will treatment affect my normal activities?
*Would a clinical trial (research study) be appropriate for me? Can you help me find one?
People do not need to ask all of their questions or understand all of the answers at one time. They will have other chances to ask the doctor to explain things that are not clear and to ask for more information.
Methods of treatment:-
The doctor is the best person to describe the treatment choices and discuss the expected results. Depending on the type and extent of the disease, patients may have chemotherapy, biological therapy, radiation therapy, or bone marrow transplantation. If the patient’s spleen is enlarged, the doctor may suggest surgery to remove it. Some patients receive a combination of treatments.
People with acute leukemia need to be treated right away. The goal of treatment is to bring about a remission. Then, when signs and symptoms disappear, more therapy may be given to prevent a relapse. This type of therapy is called maintenance therapy. Many people with acute leukemia can be cured.
Chronic leukemia patients who do not have symptoms may not require immediate treatment. The doctor may suggest watchful waiting for some patients with chronic lymphocytic leukemia. The health care team will monitor the patient’s health so that treatment can begin if symptoms occur or worsen. When treatment for chronic leukemia is needed, it can often control the disease and its symptoms. However, chronic leukemia can seldom be cured. Patients may receive maintenance therapy to help keep the cancer in remission.
A patient may want to talk to the doctor about taking part in a clinical trial, a research study of new treatment methods. The section on “The Promise of Cancer Research” has more information about clinical trials.
In addition to anticancer therapy, people with leukemia may have treatment to control pain and other symptoms of the cancer, to relieve the side effects of therapy, or to ease emotional problems. This kind of treatment is called symptom management, supportive care, or palliative care.
Chemotherapy
Most patients with leukemia receive chemotherapy. This type of cancer treatment uses drugs to kill leukemia cells. Depending on the type of leukemia, the patient may receive a single drug or a combination of two or more drugs.
People with leukemia may receive chemotherapy in several different ways:
*By mouth
*By injection directly into a vein (IV or intravenous)
*Through a catheter (a thin, flexible tube) placed in a large vein, often in the upper chest—A catheter that stays in place is useful for patients who need many IV treatments. The health care professional injects drugs into the catheter, rather than directly into a vein. This method avoids the need for many injections, which can cause discomfort and injure the veins and skin.
*By injection directly into the cerebrospinal fluid—If the pathologist finds leukemia cells in the fluid that fills the spaces in and around the brain and spinal cord, the doctor may order intrathecal chemotherapy. The doctor injects drugs directly into the cerebrospinal fluid. This method is used because drugs given by IV injection or taken by mouth often do not reach cells in the brain and spinal cord. (A network of blood vessels filters blood going to the brain and spinal cord. This blood-brain barrier stops drugs from reaching the brain.)
The patient may receive the drugs in two ways:
*Injection into the spine: The doctor injects the drugs into the lower part of the spinal column.
*Ommaya reservoir: Children and some adult patients receive intrathecal chemotherapy through a special catheter called an Ommaya reservoir. The doctor places the catheter under the scalp. The doctor injects the anticancer drugs into the catheter. This method avoids the discomfort of injections into the spine.
Patients receive chemotherapy in cycles: a treatment period, then a recovery period, and then another treatment period. In some cases, the patient has chemotherapy as an outpatient at the hospital, at the doctor’s office, or at home. However, depending on which drugs are given, and the patient’s general health, a hospital stay may be necessary.
Some people with chronic myeloid leukemia receive a new type of treatment called targeted therapy. Targeted therapy blocks the production of leukemia cells but does not harm normal cells. Gleevec, also called STI-571, is the first targeted therapy approved for chronic myeloid leukemia.
*Biological therapy
People with some types of leukemia have biological therapy. This type of treatment improves the body’s natural defenses against cancer. The therapy is given by injection into a vein.
For some patients with chronic lymphocytic leukemia, the type of biological therapy used is a monoclonal antibody. This substance binds to the leukemia cells. This therapy enables the immune system to kill leukemia cells in the blood and bone marrow.
For some patients with chronic myeloid leukemia, the biological therapy is a natural substance called interferon. This substance can slow the growth of leukemia cells.
Patients may want to ask these questions about chemotherapy or biological therapy:-
*Why do I need this treatment?
*What drugs will I get?
*Should I see my dentist before treatment begins?
*What will the treatment do?
*Will I have to stay in the hospital?
*How will we know the drugs are working?
*How long will I be on this treatment?
*Will I have side effects during treatment? How long will they last? What can I do about them?
*Can these drugs cause side effects later on?
*How often will I need checkups?
Radiation therapy
Radiation therapy (also called radiotherapy) uses high-energy rays to kill leukemia cells. For most patients, a large machine directs radiation at the spleen, the brain, or other parts of the body where leukemia cells have collected. Some patients receive radiation that is directed to the whole body. (Total-body irradiation usually is given before a bone marrow transplant.) Patients receive radiation therapy at a hospital or clinic.
These are some questions a person may want to ask the doctor before having radiation therapy:-
*Why do I need this treatment?
*When will the treatments begin? How often will they be given? When will they end?
*How will I feel during therapy? Will there be side effects? How long will they last? What can we do about them?
*Can radiation therapy cause side effects later on?
*What can I do to take care of myself during therapy?
*How will we know if the radiation is working?
*Will I be able to continue my normal activities during treatment?
*How often will I need checkups?
Stem cell transplantation:-
Some patients with leukemia have stem cell transplantation. A stem cell transplant allows a patient to be treated with high doses of drugs, radiation, or both. The high doses destroy both leukemia cells and normal blood cells in the bone marrow. Later, the patient receives healthy stem cells through a flexible tube that is placed in a large vein in the neck or chest area. New blood cells develop from the transplanted stem cells.
There are several types of stem cell transplantation:-
*Bone marrow transplantation—The stem cells come from bone marrow.
*Peripheral stem cell transplantation—The stem cells come from peripheral blood.
*Umbilical cord blood transplantation—For a child with no donor, the doctor may use stem cells from umbilical cord blood. The umbilical cord blood is from a newborn baby. Sometimes umbilical cord blood is frozen for use later.
Stem cells may come from the patient or from a donor: –
*Autologous stem cell transplantation—This type of transplant uses the patient’s own stem cells. The stem cells are removed from the patient, and the cells may be treated to kill any leukemia cells present. The stem cells are frozen and stored. After the patient receives high-dose chemotherapy or radiation therapy, the stored stem cells are thawed and returned to the patient.
*Allogeneic stem cell transplantation—This type of transplant uses healthy stem cells from a donor. The patient’s brother, sister, or parent may be the donor. Sometimes the stem cells come from an unrelated donor. Doctors use blood tests to be sure the donor’s cells match the patient’s cells.
*Syngeneic stem cell transplantation—This type of transplant uses stem cells from the patient’s healthy identical twin.
After a stem cell transplant, patients usually stay in the hospital for several weeks. The health care team protects patients from infection until the transplanted stem cells begin to produce enough white blood cells.
These are some questions a person may want to ask the doctor before having a stem cell transplant:-
*What kind of stem cell transplant will I have? If I need a donor, how will we find one?
*How long will I be in the hospital? What care will I need when I leave the hospital?
*How will we know if the treatment is working?
*What are the risks and the side effects? What can we do about them?
*What changes in normal activities will be necessary?
*What is my chance of a full recovery? How long will that take?
*How often will I need checkups?
Click to see the side effect of Leukemia treatment
Click to see :->Leukemia and Treatment options for leukemia by type
What happens after treatment for leukemia.
What does the future hold for patients with leukemia.
Disclaimer: This information is not meant to be a substitute for professional medical advise or help. It is always best to consult with a Physician about serious health concerns. This information is in no way intended to diagnose or prescribe remedies.This is purely for educational purpose.
Resources:
http://www.medicinenet.com/leukemia/article.htm
http://www.nortonhealthcare.com/specialties/cancer/leukemia/leukemia.aspx
![Reblog this post [with Zemanta]](https://i0.wp.com/img.zemanta.com/reblog_e.png?w=580)



















